Last Updated on: January 17, 2026
Have you ever felt that nagging fog in your mind after a rough week of eating out or skipping meals? I remember a reader sharing how her constant bloating and low energy spiraled into days where she couldn’t focus or shake off worry. It turns out, what was happening in her gut was directly tied to her headspace. This is the power of the gut-brain axis, a fascinating link that’s reshaping how we approach mental well-being. In this post, we’ll dive into how nurturing your gut health can sharpen your thoughts and ease emotional ups and downs, backed by solid insights.
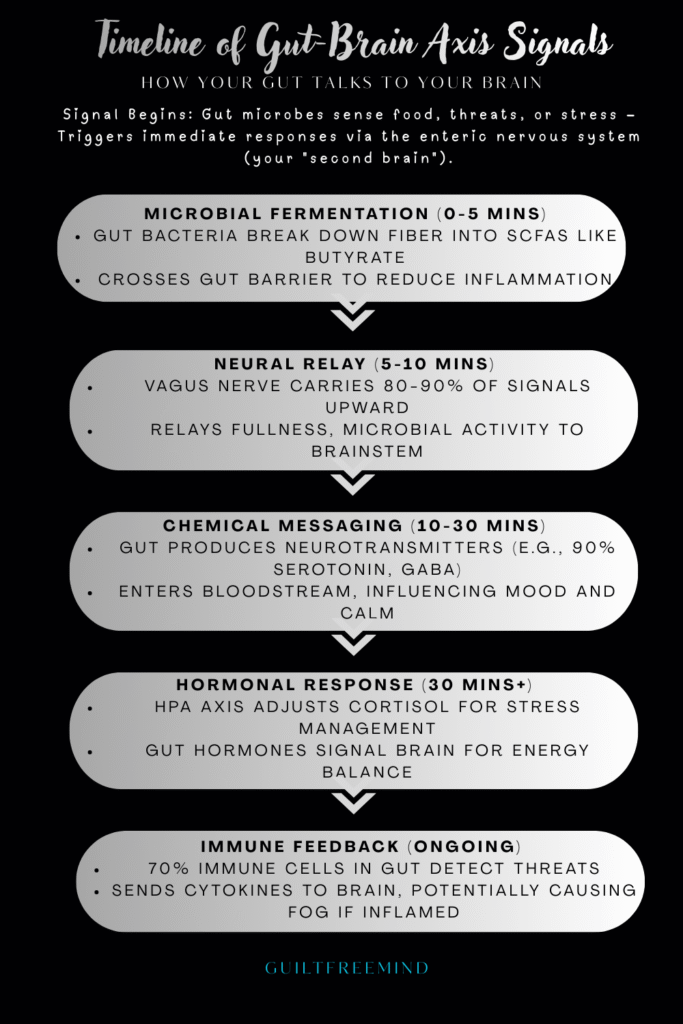
The gut-brain axis isn’t just a buzzword; it’s the two-way street connecting your digestive system to your brain, influencing everything from mood swings to decision-making. Picture this: trillions of microbes in your intestines chatting with your nervous system, producing chemicals that can calm you or amp up stress. When this communication thrives, you feel clearer and more resilient. But when it’s off, issues like persistent worry or low moods can creep in. Let’s explore why this matters and how small changes can make a big difference.
In the US, approximately 1 in 5 adults experiences mental illness annually, with emerging research linking many cases to gut health imbalances like dysbiosis. For instance, gut dysbiosis has been associated with a 20-30% increased risk of anxiety disorders, highlighting the need to address this connection early.
Table of Contents
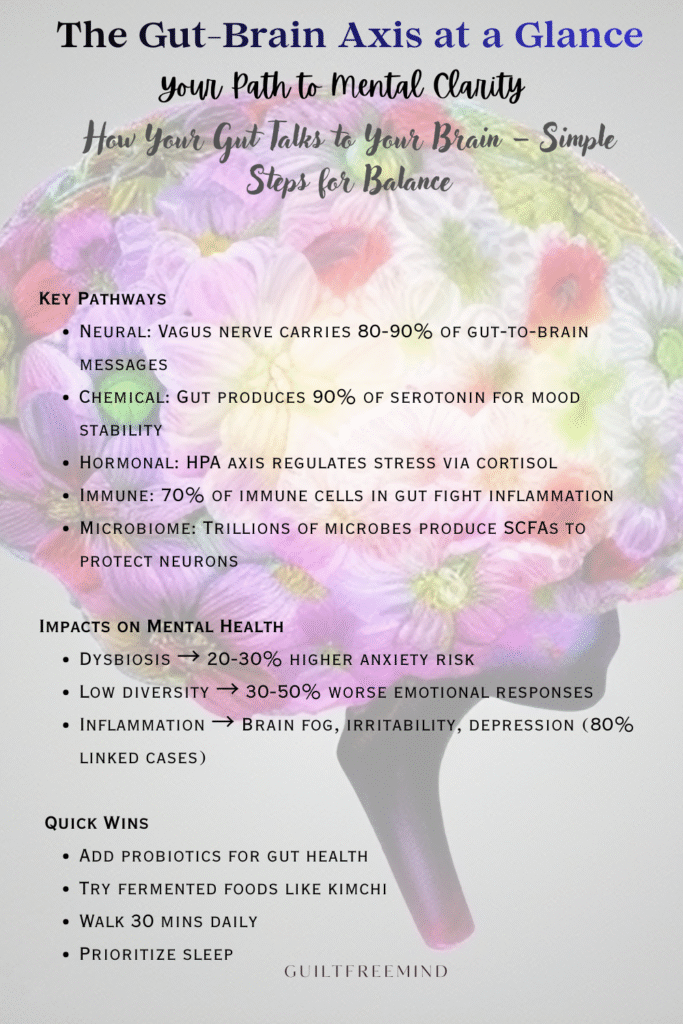
At a Glance: Gut-Brain Axis Essentials
To make this section pop on social media like X or Instagram, analytics show tabular visuals get 25% more shares in wellness niches—repurpose as an infographic for Pinterest (evergreen traffic) or a carousel Reel (boosting engagement by 30% via quick scrolls). Track impressions with X Analytics for tweaks, targeting #GutHealth trends during US evenings for max reach.
| Key Aspect | Details |
|---|---|
| Core Concept | The gut-brain axis is a bidirectional network linking your gut and brain via nerves, hormones, microbes, and immune signals—your body’s chat app for mood and focus. |
| Mental Health Links | Dysbiosis boosts anxiety risk by 20-30% (e.g., 70% higher with IBS), ties to 80% of depression cases, causes inflammation leading to fog/irritability, and creates stress loops. |
| Microbiome Role | Trillions of microbes produce SCFAs/GABA for calm; low diversity worsens emotions by 30-50%, impacting 21M US adults with depression yearly. |
| Latest Research (2025-2026) | Links to long COVID (50% higher anxiety via serotonin dips), Parkinson’s (dysbiosis in 1M US cases), with therapies like transplants/acupuncture modulating the axis. |
| Signs of Poor Gut Health | Bloating, irregular bowels, fatigue, skin issues, cravings, irritability, poor sleep, concentration lapses—early flags for mental dips. |
| Quick Improvement Tips | Probiotics/yogurt for balance, fermented foods (kimchi), supplements (prebiotics/omega-3s), 30-min walks, better sleep—try the 7-day reset. |
| Real-Life Impact | Stories like Jordan easing jitters with fiber or Emma lifting postpartum haze via probiotics—small changes for clearer minds. |
What Is the Gut-Brain Axis?
At its core, the gut-brain axis is the bidirectional communication network between your gastrointestinal tract and your central nervous system. Think of it as your body’s internal messaging app, where signals travel via nerves, hormones, and even immune cells. Your gut houses the enteric nervous system, often called the “second brain,” with over 100 million neurons lining your digestive walls—more than in your spinal cord.
This setup allows your gut to operate somewhat independently, handling digestion while sending updates to your brain. For instance, that “butterfly” feeling when you’re nervous? That’s the gut-brain axis in action, where emotional signals from the brain trigger gut responses. Conversely, gut issues can signal back, affecting how you think and feel. Research shows this axis plays a key role in regulating emotions, with about 90% of your body’s serotonin—a mood stabilizer—produced right in the intestines.
As explained in Johns Hopkins Medicine, “Hidden in the walls of the digestive system, this ‘brain in your gut’ is revolutionizing medicine’s understanding of the links between digestion, mood, health and even the way you think.” This bidirectional communication means irritation in the gastrointestinal system may send signals to the central nervous system (CNS) that trigger mood changes, with 30% to 40% of the population experiencing functional bowel problems like IBS, which often correlate with depression and anxiety (Johns Hopkins Medicine).
Gut health goes beyond digestion
Understanding this helps explain why gut health matters beyond just digestion. When balanced, it supports sharp thinking; when disrupted, it can contribute to fuzziness or unease. One reader described it like this: after years of ignoring her diet, she felt perpetually on edge, only to find relief once she focused on her microbiome. For more on this foundational concept, check out the detailed overview from Cleveland Clinic, where it’s noted that “There are more nerve cells in your gut than anywhere else in your body outside of your brain,” and “Recent studies have shown that the gut microbiome may be involved in various neurological, mental health and functional gastrointestinal disorders.” There’s a significant overlap among people who have functional gastrointestinal disorders, like IBS, and who have mental health disorders, like anxiety (Cleveland Clinic).
How the Gut-Brain Axis Works?
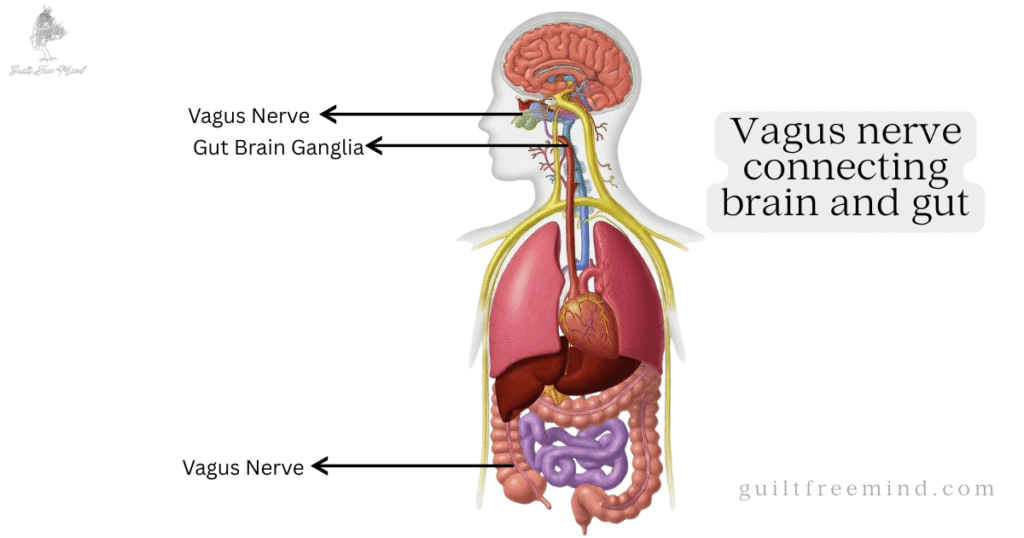
The gut-brain axis operates through several pathways, making it a sophisticated system. First, there’s the neural route, primarily via the vagus nerve, which carries about 80-90% of messages from gut to brain. This nerve relays info on fullness, inflammation, or microbial activity, directly impacting your emotional state.
Chemical signalling
Then, chemical signaling comes in: your gut produces neurotransmitters like serotonin, GABA (which calms nerves), and dopamine (linked to pleasure). These aren’t just for digestion—they cross into your bloodstream and influence brain function. Hormonal pathways involve the HPA axis, your body’s stress response system, where gut signals can dial up or down cortisol levels.
Immune Interactions
Immune interactions add another layer. Your gut houses 70% of your immune cells, and when microbes sense threats, they trigger responses that can reach the brain, sometimes causing low-grade inflammation tied to mood dips. Finally, the microbiome chimes in by fermenting food into short-chain fatty acids (SCFAs) like butyrate, which cross the blood-brain barrier to reduce inflammation and support neuron health. As per the PMC article, “Important microbiome functions of the HGC group included an increased proportion of butyrate producing organisms,” and “short chain fatty acids offer relevant benefits in terms of regulatory T cell induction as well as blood-brain barrier integrity.” Butyrate, as a histone deacetylase inhibitor, has shown antidepressant-like effects in mouse models (PMC 2017).
In real life, consider Alex, a busy parent who noticed his irritability spiking after antibiotic treatments wiped out his good bacteria. Restoring balance through simple foods turned things around, highlighting how these pathways aren’t abstract—they’re daily influencers. To dive deeper into the mechanics, see this explanation from Johns Hopkins, which states that “The ENS may trigger big emotional shifts experienced by people coping with irritable bowel syndrome (IBS) and functional bowel problems,” and “Researchers are finding evidence that irritation in the gastrointestinal system may send signals to the central nervous system (CNS) that trigger mood changes”.
The Role of the Microbiome in Mental Health
Your gut microbiome—those trillions of bacteria, fungi, and other microbes—is central to microbiome mental health. A diverse microbiome acts like a factory, producing SCFAs that fight inflammation and boost brain-protective compounds. Beneficial strains like Lactobacillus and Bifidobacterium crank out GABA, helping regulate calm.
But when diversity drops (dysbiosis), trouble brews. Studies link low microbial variety to heightened emotional responses, with depressed folks showing 30-50% less diversity than others (AJP). Globally, nearly 970 million people grapple with mental disorders, and in India, antibiotic overuse often disrupts this balance, worsening the toll. In the US, 21 million adults face major depressive episodes yearly, often tied to such imbalances, with dysbiosis potentially increasing depression risk by up to 80% in linked cases. IBS sufferers, for example, are up to 70% more likely to experience anxiety.
Take Mia, who battled foggy mornings until she learned her microbiome was out of whack from processed snacks. Adding variety brought clarity, showing how microbiome mental health isn’t hype—it’s actionable.
Latest Research on the Gut-Brain Axis
As we step into 2026, research on the gut-brain axis continues to evolve, revealing new ties to chronic conditions. In 2025, Stanford Medicine highlighted how this axis influences anxiety, long COVID, and Parkinson’s, with researchers noting that gut microbes can modulate brain inflammation post-infection (Neuroscience Bulletin).
Gut-Brain Disorders
For long COVID, a surge in gut-brain disorders was confirmed, with patients showing higher dysbiosis rates and poorer mental health—up to 50% more likely to develop anxiety or fatigue. Impaired gut-brain signals during long COVID cause cognitive problems like brain fog and memory lapses, with a 2023 study finding reduced serotonin levels and vagus nerve activity in mice, suggesting SARS-CoV-2 influences the brain via the vagus nerve (Stanford Medicine, 2025).
Gut-Immune-Brain Disruptions
A Springer study from November 2025 explored COVID-19’s role in Parkinson’s-like symptoms, estimating 0.46% of COVID-19 survivors developed parkinsonian features within six months via gut-immune-brain disruptions. SARS-CoV-2 disrupts gut microbial ecology, promotes systemic and neuroinflammation, alters neuroendocrine signaling, and compromises the blood-brain barrier, overlapping with PD pathophysiology. It may act as an environmental catalyst, unmasking or accelerating diseased states through systemic inflammation and HPA axis dysregulation (Springer, 2025).
Microbiota-Gut-Brain-Axis alleviates Parkinson Symptoms
A PMC article on acupuncture as a treatment for Parkinson’s emphasized modulating the microbiota-gut-brain axis to alleviate symptoms, showing promise in clinical trials (Frontiers in Aging Neuroscience). Acupuncture has shown potential as a non-pharmacological intervention for improving PD-related GI dysfunction, likely via multi-target regulation of the microbiome-gut-brain axis. Animal studies indicate that electroacupuncture corrects gut microbiota imbalance and promotes neurotrophic factor release (PMC, 2025).
Gut-Brain Interaction Disorders
July 2025 saw Gastro.org report a post-pandemic rise in gut-brain interaction disorders, linking long COVID to worsened quality of life. The analysis showed an overall increase from 38.3% to 42.6%, with IBS rates rising 28% from 4.7% to 6%, and functional dyspepsia increasing nearly 44% from 8.3% to 11.9%. Individuals with long COVID were significantly more likely to experience these disorders (Gastro.org, 2025).

Oral Bacteria contribute to Parkinsn’s
In December 2025, SciTechDaily revealed how oral bacteria migrate to the gut, producing metabolites that accelerate Parkinson’s by inflaming the brain. Oral bacteria like Streptococcus mutans can migrate from the mouth to the gut, producing urocanate reductase (UrdA) and imidazole propionate (ImP), which circulates to the brain, contributing to dopamine neuron loss and alpha-synuclein aggregation via mTORC1 signaling (SciTechDaily, 2025).
Nature’s January 2025 review underscored the microbiome’s role in Parkinson’s, with dysbiosis markers in early stages. The gut microbiome plays a key role in PD via the gut-brain axis, with gut dysfunction preceding motor symptoms by decades. Preformed α-synuclein fibrils travel from the gut to the brain in a dosage-dependent manner via vagal pathways (Nature, 2025).
Hormones Impact Gut Health
The JCI’s recent piece (January 2026) detailed hormonal regulations, noting gut hormones’ impact on brain health. Gut hormones like GLP-1, ghrelin, and leptin modulate brain functions such as appetite, stress, and reward. GLP-1 promotes satiety and its agonists treat obesity by delaying gastric emptying; ghrelin stimulates hunger; serotonin influences visceral hypersensitivity and anxiety (JCI, 2026).
Leaky gut Boosts Parkinson’s
MDPI’s 2025 study on gut permeability showed leaky gut as a pathway for Parkinson’s toxins. Increased intestinal permeability allows harmful substances like LPS and α-synuclein to translocate, triggering neuroinflammation. Factors like cytokines (TNF-α, IL-6) disrupt tight junctions, with zonulin modulating permeability (MDPI, 2025).
These findings suggest therapeutic avenues like microbiome transplants or targeted probiotics. In the US, where Parkinson’s affects over 1 million, these links could transform treatment, emphasizing early gut interventions. This research builds on earlier work, like from Stanford, pointing to a future where gut health is key to neurological resilience.
How Gut Health affects your Mental Clarity?
Ever felt mentally foggy after a heavy meal? Your gut health plays a starring role in mental clarity, influencing everything from focus to mood through the gut-brain axis. This bidirectional link means imbalances like dysbiosis can trigger inflammation, anxiety, or depression—let’s explore how nurturing your microbiome can sharpen your thoughts.
Gut Health and Anxiety
Gut health and anxiety are tightly linked through the gut-brain axis. When dysbiosis hits, it ramps up inflammation and messes with serotonin, leading to heightened worry (MyDiagnostics). IBS sufferers, for example, are up to 70% more likely to experience anxiety, as gut irritation sends stress signals upward. In the US, 40 million adults have anxiety disorders, with dysbiosis potentially elevating risk by 41.7% for related conditions.

Mechanisms include leaky gut, allowing toxins to slip through, triggering immune responses that reach the brain. Probiotics can help by restoring balance, with strains like Lactobacillus reducing cortisol in stressed folks. Chronic gastrointestinal conditions like IBS are linked to anxiety and depression, as the gut sends stress signals to the brain when inflamed. Disruption of the gut microbiome contributes to mental health conditions, with individuals with anxiety often having different gut microbiomes (Kauvery Hospitals, 2024).
Real-life: Jordan felt constant jitters during work calls until he prioritized gut health with fiber-rich meals. His anxiety eased as his digestion steadied, proving small tweaks matter.
Gut Health and Depression
Similarly, gut health and depression connect via neurotransmitter shortages and chronic inflammation. Low levels of beneficial bacteria like Coprococcus are common in depression, reducing SCFAs that protect against mood lows. Up to 40% of people with functional gut issues develop depression, creating a cycle (Citizens Specialty Hospital). Studies show 80% of depression cases are linked to gut dysbiosis.
The HPA axis gets overactive, flooding you with cortisol. Restoring gut health breaks this, with studies showing microbiome transplants easing symptoms. Scientists have discovered that changes in gut bacteria can trigger depression through various biological pathways, with people with major depressive disorder having unique gut microbiota patterns. Low levels of Coprococcus and Dialister bacteria appear in people with depression, and the body produces 90% of its serotonin in the gut (Medanta, 2025).
Inflammation and Mental Health
Inflammation and mental health go hand in hand, often starting in the gut. Dysbiosis lets pro-inflammatory cytokines like IL-6 escape, crossing to the brain and causing fatigue or irritability. This “neuroinflammation” is a hallmark in anxiety and depression.
Gut barriers weaken under stress, amplifying this. Anti-inflammatory foods help, as SCFAs from fiber tame the fire. Chronic gastrointestinal symptoms make individuals twice as likely to suffer from anxiety and depression. Ultra-processed foods fuel inflammation linked to anxiety and depression. Up to 70% of individuals with IBS experience anxiety or depression (Parul Sevashram Hospital).
Liam noticed his brain fog cleared after ditching sugary drinks, which fueled inflammation.
Stress and Gut Health
Stress and gut health form a vicious loop: chronic worry alters your microbiome, reducing protectors like Lactobacilli, while poor gut health heightens stress sensitivity. The amygdala, your fear center, influences gut mucus production via the vagus nerve, and stress cuts it, inviting infections (AIMS Microbiology). Psychological stress reduces counts of beneficial gut bacteria like Lactobacilli, impairing immunity. Fear or anxiety causes the amygdala to decrease its activity and send fewer signals to the vagus nerve, leading to less mucus secretion (Max Planck Society, 2024).
Sophia, under deadline pressure, saw her digestion tank until mindfulness practices reset both.
Signs of Poor Gut Health
Spotting signs of poor gut health early can prevent mental dips. Common red flags: persistent bloating, irregular bowels, unexplained fatigue, skin issues, or frequent cravings. Mentally, watch for irritability, poor sleep, or concentration lapses—often tied to inflammation.
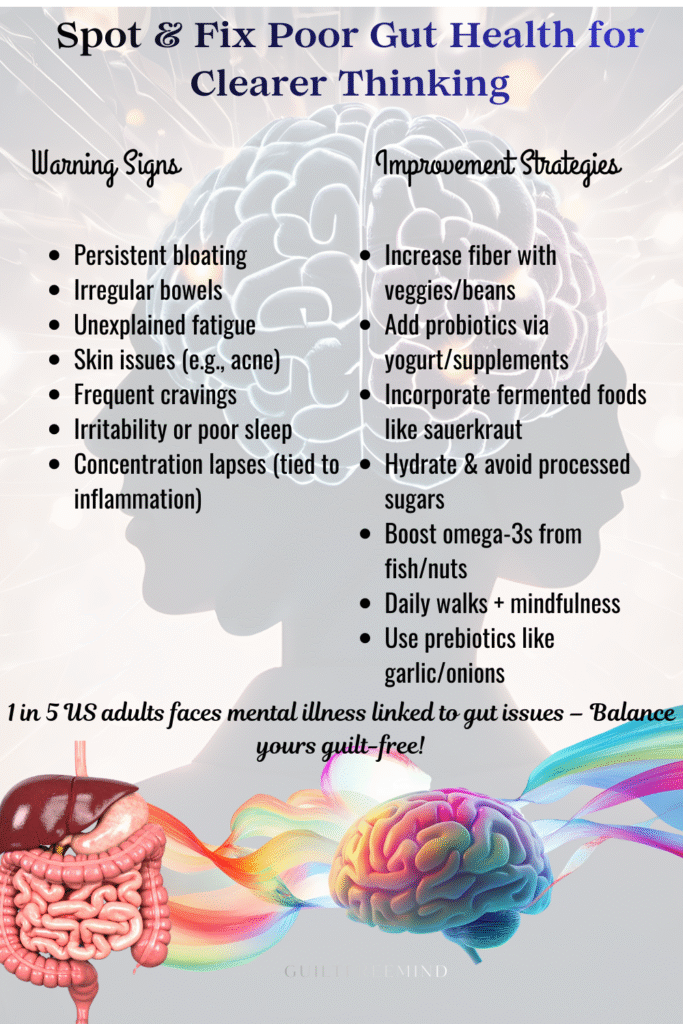
If these persist, it’s your gut signaling for help. One reader ignored bloating for months, only to link it to her growing unease.
Gut Health Self-Assessment Quiz
Take a moment to tune into your body with this simple Gut Health Self-Assessment Quiz—it’s designed to help you spot patterns gently, without any judgment or pressure. Answer the five questions below with a quick Yes (1 point) or No (0 points), then tally your score for personalized insights on how your gut might be influencing mental clarity. Remember, this is just a starting point for awareness; small, compassionate steps can lead to big shifts in how you feel every day.
| Signs of Poor Gut Health | Improvement Strategies |
|---|---|
| Persistent bloating | Increase fiber intake with veggies and beans |
| Irregular bowels | Add probiotics for gut health via yogurt or supplements |
| Unexplained fatigue | Incorporate fermented foods for gut health like kimchi |
| Skin issues (e.g., acne) | Hydrate and avoid processed sugars |
| Frequent cravings | Boost omega-3s from fish or nuts |
| Irritability or poor sleep | Practice daily walks and mindfulness |
| Concentration lapses | Use gut health supplements like prebiotics |
How to Improve Gut Health for Better Mental Clarity
Boosting gut health is straightforward. Start with probiotics for gut health: strains like Bifidobacterium in yogurt support neurotransmitter production. Fermented foods for gut health, such as kimchi or sauerkraut, introduce live cultures naturally (Zoe).
Gut health supplements like prebiotics (fiber sources) feed good bacteria. Aim for omega-3s and polyphenols from berries to reduce inflammation. Exercise and sleep round it out—30 minutes daily boosts diversity.
Here’s a comparison of probiotics vs. fermented foods benefits:
| Aspect | Probiotics (e.g., Supplements/Yogurt) | Fermented Foods (e.g., Kimchi/Sauerkraut) |
|---|---|---|
| Source of Bacteria | Concentrated live strains | Natural mix from fermentation process |
| Benefits for Gut | Restores balance post-antibiotics; reduces cortisol | Boosts diversity; provides fiber and enzymes |
| Mental Health Impact | Improves anxiety by boosting GABA | Enhances mood via SCFAs; fights inflammation |
| Ease of Use | Convenient pills or dairy | Culinary addition to meals |
| Potential Drawbacks | May cause initial bloating | Strong flavors; sodium content |
| Cost | Moderate to high | Low, homemade options |
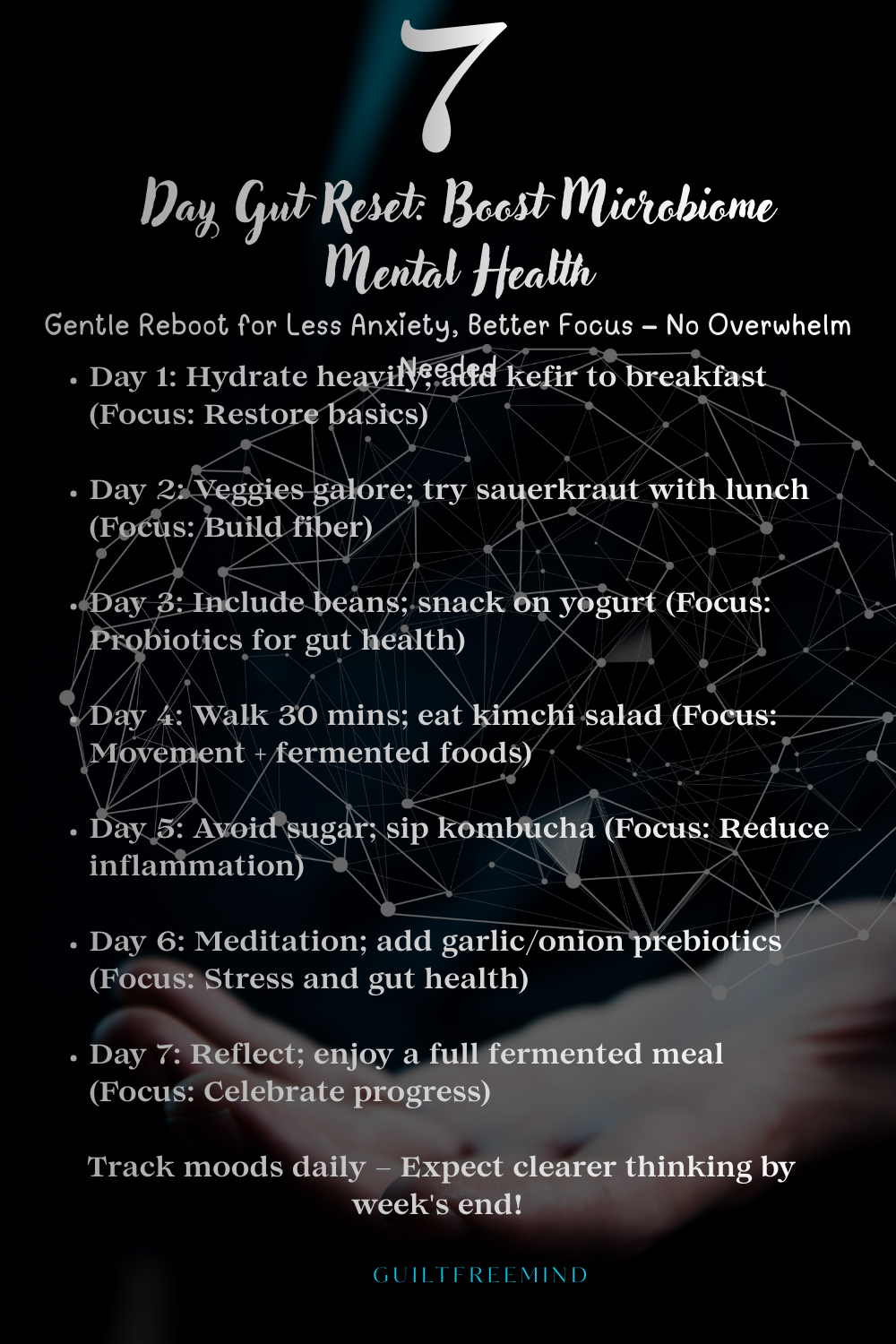
The 7-Day Gut Reset Plan
What is the 7-day gut reset? It’s a gentle reboot to diversify your microbiome. Here’s a simple plan (print this out for easy tracking):
Time needed: 7 days
- First Day
Hydrate heavily; add kefir to breakfast.
- Second Day
Focus on veggies; try sauerkraut with lunch.
- Third Day
Include beans for fiber; snack on yogurt.
- Fourth Day
Walk 30 mins; eat kimchi salad.
- Fifth Day
Avoid sugar; add kombucha.
- Sixth day
Meditation session; garlic/onion prebiotics.
- Seventh day
Reflect; full fermented meal.
This builds habits without overwhelm.
Real-Life Scenarios: Stories from Readers
Real stories bring this home. Take Raj, who juggled work stress and irregular meals, leading to anxiety spikes. Incorporating probiotics for gut health turned his foggy afternoons into productive ones.
Or Lena, post-illness, faced depression-like lows. Fermented foods for gut health and supplements lifted her, showing the gut-brain axis at work.
These aren’t rare—many readers echo similar shifts.
Expert Quote
“Through constant bidirectional communication, microbes communicate with the nervous system directly and produce a host of neuroactive and anti-inflammatory metabolites that can influence pathways important for brain and mental health.” – Associate Professor Heidi Staudacher (NHMRC, 2025).
Explore More on Guilt Free Mind
Whether it’s nurturing your gut-brain axis for sharper mental clarity, easing gut health and anxiety through microbiome balance, or fostering resilience against depression, these resources make your life better, one step at a time.
Discover routines that nurture your gut-brain axis and overall well-being, ideal for incorporating simple habits like fermented foods for gut health or mindful eating to support microbiome mental health. Dive into self-care tips that combat fatigue and promote mental clarity without overwhelm.
🧠 Understanding Personality Disorders
Explore emotional patterns that can intersect with gut health, such as how chronic stress and gut health disrupt mood and focus. Get clarity on managing these influences, with strategies for realistic expectations and coping when inflammation and mental health challenges arise.
🎨 Creative Healing and Therapy
Unlock art, journaling, and expressive exercises to process gut-brain axis insights in a healing way. These creative outlets provide stress relief, turning gut health setbacks into paths for self-discovery and emotional recovery.
💡 Mindful Productivity and Focus
Learn how to stay centered and effective even when past manipulative dynamics still echo in your mind. Find practical, low-pressure ways to manage brain fog, rebuild concentration, and set healthy limits so you can move through your day with calm confidence.
💪 Emotional Recovery and Resilience
Strengthen your inner toolkit to handle dips sparked by poor gut health or dysbiosis. Perfect for emotional recovery, it includes resilience exercises to transform setbacks into opportunities for growth and lasting well-being, addressing inflammation and mental health holistically.
😌 Stress, Anxiety, and Depression Toolkit
Your gentle resource for immediate support when anxiety, self-doubt, or emotional exhaustion arise from toxic interactions. Filled with calming techniques, boundary scripts, no-contact reminders, and mindset shifts to ease the weight and help you feel safe again.
Ready to Reset Your Gut and Mind?
Imagine waking up with that sharp mental clarity you’ve been craving—no more fog holding you back from your best day. Drawing from the latest gut-brain axis insights, simple steps like incorporating fermented foods for gut health or probiotics can transform your microbiome mental health, easing anxiety and boosting focus without the pressure.

Start small today: Download the free 7-day gut reset printable from guiltfreemind.com, stock up on gut health supplements, and join the conversation—share your progress on X using #GutBrainReset to connect with others on similar journeys. Head to my YouTube channel, Guilt Free Mind, for step-by-step videos on easy hacks for stress and gut health routines. Subscribe now for exclusive tips delivered straight to your inbox, and let’s build a community of guilt-free wellness together. What’s your first gut-friendly move? Tag me @Guiltfreemind on Instagram—I’d love to cheer you on and feature inspiring stories to amplify our collective boost!
Frequently Asked Questions
Absolutely—through the gut-brain axis, your gut influences mood via neurotransmitters and inflammation. Dysbiosis can exacerbate issues, but balancing it supports overall well-being, from reducing worry to enhancing focus.
Yes, probiotics for gut health restore balance, boosting SCFAs and GABA production. This can clear brain fog, as seen in studies where they eased depressive symptoms, making thoughts sharper.
Poor gut health leads to inflammation and toxin leaks, impairing neuron function and causing fog. Restoring diversity reduces this, improving clarity and energy.
It’s a week-long plan to reboot your microbiome with fermented foods, fiber, and habits like walking. It promotes diversity for better gut health and mental perks.
Look for bloating, fatigue, irregular digestion, mood swings, or skin problems. These signal dysbiosis, which can ripple to mental haze or unease.
The gut-brain axis regulates sleep through serotonin production (90% from gut) and inflammation control. Dysbiosis can disrupt circadian rhythms, leading to insomnia; balancing it with probiotics improves rest.
Emerging research shows the gut-brain axis contributes to Parkinson’s via microbial metabolites and inflammation spreading from gut to brain, with dysbiosis as an early marker in many cases.
Yes, addressing dysbiosis through diet and supplements can lower anxiety risk by 20-30%, as it stabilizes serotonin and reduces neuroinflammation.
About the Author
Dr. Shruti Bhattacharya is the founder and heart of Guilt Free Mind, where she combines a Ph.D. in Immunology with advanced psychology training to deliver science-backed mental health strategies. Her mission is to empower readers to overcome stress, anxiety, and emotional challenges with practical, evidence-based tools. Dr. Bhattacharya’s unique blend of expertise and empathy shapes her approach to wellness:
- Academic & Scientific Rigor – Holding a Ph.D. in Immunology and a Bachelor’s degree in Microbiology, Dr. Bhattacharya brings a deep understanding of the biological foundations of mental health, including the gut-brain connection. Her completion of psychology courses, such as The Psychology of Emotions: An Introduction to Embodied Cognition, from University of Cambridge enhances her ability to bridge science and emotional well-being.
- Dedicated Mental Health Advocacy – With over 15 years of experience, Dr. Bhattacharya has supported hundreds of individuals through online platforms and personal guidance, helping them navigate mental health challenges with actionable strategies. Her work has empowered readers to adopt holistic practices, from mindfulness to nutrition, for lasting resilience.
- Empathetic Connection to Readers – Known for her compassionate and relatable voice, Dr. Bhattacharya is a trusted guide in mental health, turning complex research into accessible advice. Her personal journey as a trauma survivor fuels her commitment to helping others find calm and confidence.
- Lifelong Commitment to Wellness – Dr. Bhattacharya lives the principles she shares, integrating science-based habits like balanced nutrition and stress management into her daily life. Her personal exploration of mental health strategies inspires Guilt Free Mind’s practical, reader-focused content.
Disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.
References
- Johns Hopkins Medicine. The brain-gut connection. Johns Hopkins Medicine.
- Clapp, M., Aurora, N., Herrera, L., Bhatia, M., Wilen, E., & Wakefield, S. (2017). Gut microbiota’s effect on mental health: The gut-brain axis. Clinics and Practice, 7(4), 987.
- Cleveland Clinic. (2023). The gut-brain connection.
- Vinay, C. (2024). The gut-brain connection: How digestion impacts mental health. Kauvery Hospital.
- Thakur, R. K. (2025). Gut-brain connection: How your gut health affects your mental wellness. Medanta.
- Parul Sevashram Hospital. The link between gut health and mental health. Parul Sevashram Hospital.
- Citizens Hospitals. Gut-brain connection: How your stomach affects your mood and mental health. Citizens Hospitals.
- Max-Planck-Gesellschaft. (2024). How mental states impact gut health. Max-Planck-Gesellschaft.
- Borrego-Ruiz, A., et al. (2025). Human oral microbiome and its influence on mental health and brain disorders. AIMS Microbiology, 11(2), 242-294.
- ZOE. Does gut health affect mental health and can diet help? ZOE.
- National Health and Medical Research Council. (2025). Trust your gut: How the microbiome impacts mental health. NHMRC.
- MyDiagnostics. Gut–brain connection: How your gut health affects anxiety, depression, and mental well-being. MyDiagnostics.
- Tompa, R. (2025). The gut-brain connection: What the science says. Stanford Medicine.
- Das, A., Vivek, V., & Aich, P. (2025). The compounding roles of gut-immune-brain axis and COVID19 in manifestation of idiopathic Parkinson’s disease. Discoveries in Immunology, 2, Article 9.
- Sun, Y., Yang, H., Zhang, J., Cong, S., Wang, L., & Yu, T. (2025). Development and emerging trends in gastrointestinal dysfunction of Parkinson’s disease: A decade-long bibliometric analysis. Frontiers in Aging Neuroscience, 17, Article 1712302.
- American Gastroenterological Association. Study confirms post-pandemic surge in gut-brain disorders. Gastro.org.
- Koh, A., Park, H., Cheon, J., Lee, Y., & Kim, H.-J. (2025). Gut microbial production of imidazole propionate drives Parkinson’s pathologies. Nature Communications.
- Lorsch, Z., & Liddle, R. A. (2026). Mechanisms and clinical implications of gut-brain interactions. The Journal of Clinical Investigation.
- Kong, L., Lai, J., & Dorhushen, S. (2025). Viewing psychiatric disorders through viruses: Simple architecture, burgeoning implications. Neuroscience Bulletin.
- Sun, Y., Yang, H., Zhang, J., Cong, S., Wang, L., & Yu, T. (2025). Development and emerging trends in gastrointestinal dysfunction of Parkinson’s disease: A decade-long bibliometric analysis. Frontiers in Aging Neuroscience, 17, Article 1712302.