Last Updated on: December 20, 2024
Depression can feel like a heavy fog, clouding your thoughts and draining your energy. As a mental health blogger at Guilt Free Mind, I’ve seen how this condition affects my readers, often accompanied by overwhelming guilt. Cognitive behavioral therapy for depression is a powerful tool to lift that fog, helping you reframe negative thoughts and rediscover joy. In this article, I’ll guide you through how cognitive behavioral therapy for depression works, share practical strategies, and provide real-life scenarios to show its impact. Whether you’re struggling with persistent sadness or guilt, this post will equip you with actionable steps to start your journey toward a guilt-free mind.
Table of Contents
At a Glance
| Category | Quick Insight |
|---|---|
| Overview | Cognitive Behavioral Therapy (CBT) is a structured, evidence-based psychotherapy that manages depression by addressing negative thought patterns and behaviors. Effective for mild to moderate depression, with up to 60% symptom improvement and 50% lower relapse rates vs. medication alone [AAFP]. |
| Key Techniques | – Cognitive Restructuring: Reframe negative thoughts (e.g., “I’m worthless” to “I’m capable”) in 10-15 min/day. – Behavioral Activation: Schedule enjoyable activities (5-30 min). – Thought Journaling: Track thoughts/emotions to identify patterns (10-20 min). – Mindfulness-Based CBT: Focus on breath to reduce rumination (5-15 min). |
| Effectiveness | – Backed by 106+ studies, with a 1.97 standardized mean symptom change [PMC]. – Comparable to antidepressants for mild/moderate depression [APA]. – Reduces guilt, especially in postpartum depression [Healthline]. |
| Who It’s For | Adults, adolescents, diverse populations (e.g., India, US). Ideal for guilt, rumination, or sadness. |
| How to Start | – Self-Help: Use CBT worksheets, journal, or practice mindfulness. – Professional Help: In-person ($100-$200/session) or online therapy ($60-$120/session) via BetterHelp or Psychology Today. |
| Why It Works | Targets the cognitive triad (negative views of self, world, future) with practical, skill-based tools for resilience [BPS Medicine]. |
| Resources | Explore Guilt Free Mind’s blog for CBT worksheets and mindfulness tips [Link Placeholder]. |
| Author | Dr. Shruti Bhattacharya, Ph.D. in Immunology, blends science and psychology for actionable mental health strategies. Featured in Feedspot’s Top 100 Mental Health Blogs (2025). |
| Last Updated | August 15, 2024 |
| Disclaimer | This content is for informational purposes only and not a substitute for professional medical advice. |
What Is Cognitive Behavioral Therapy for Depression?
Cognitive behavioral therapy for depression is a structured, goal-oriented form of psychotherapy that focuses on changing negative thought patterns and behaviors. Unlike traditional talk therapy, it’s short-term (typically 5-20 sessions) and emphasizes practical skills you can apply daily. Developed by Dr. Aaron Beck in the 1960s, it’s based on the idea that thoughts, feelings, and behaviors are interconnected. By addressing distorted thoughts, cognitive behavioral therapy for depression helps you break the cycle of negativity that fuels low mood.

For example, if you think, “I’m a failure,” cognitive behavioral therapy for depression teaches you to challenge that belief and replace it with a more balanced perspective, like, “I made a mistake, but I’m learning.” It’s evidence-based, with studies showing it’s as effective as antidepressants for mild to moderate depression, and it reduces relapse rates by up to 50% AAFP.
Why Cognitive Behavioral Therapy for Depression Works
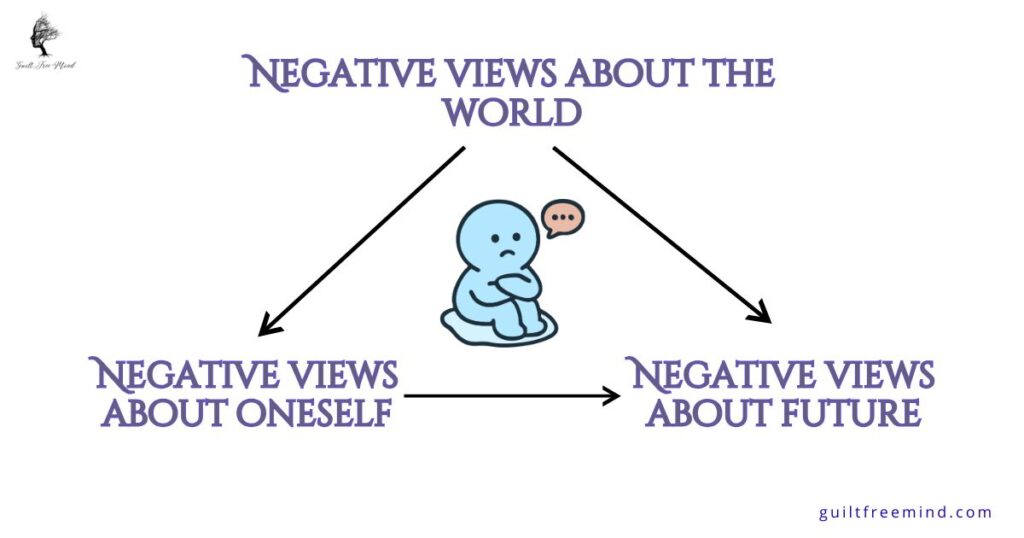
Cognitive behavioral therapy for depression targets the root of depressive symptoms: distorted thinking. It’s built on the “cognitive triad,” which suggests depression stems from negative views of yourself, the world, and the future. By restructuring these thoughts, cognitive behavioral therapy for depression empowers you to take control of your emotions. It’s effective because it’s:
- Structured: Sessions follow a clear plan, with homework to reinforce skills.
- Practical: You learn tools like journaling and behavioral activation to use in everyday life.
- Evidence-Based: Over 106 studies show its efficacy for depression, with face-to-face CBT achieving a standardized mean change of 1.97 in symptoms.
CBT targets the root of depression by rewiring negative thought patterns, offering lasting tools for resilience beyond medication.
Dr. Aaron T. Beck, psychiatrist and CBT founder Beck Institute
Globally, depression affects over 300 million people, with cognitive behavioral therapy for depression showing promise in countries like India PMC. In the US, over 21 million adults face depression yearly, making CBT a vital tool APA.
Real-Life Scenario
Meet Sarah, a 32-year-old teacher who felt trapped in a cycle of sadness and self-doubt. She often thought, “I’m not good enough for my students,” which led to withdrawing from social activities. After starting cognitive behavioral therapy for depression, Sarah worked with her therapist to identify these thoughts as “all-or-nothing” thinking. Using cognitive restructuring, she replaced them with, “I’m doing my best, and my students appreciate my effort.” She also practiced behavioral activation by scheduling coffee dates with friends, which lifted her mood. Within 12 weeks, Sarah felt more confident and reconnected with her passion for teaching.
Sarah’s story shows how cognitive behavioral therapy for depression can transform lives by addressing both thoughts and actions. It’s not about “thinking positive” but about thinking realistically.
Cognitive behavioral therapy enhances brain circuits to relieve depression, with certain neural changes predicting which patients benefit most from problem-solving approaches.
– Dr. Leanne Williams, Stanford psychiatrist.
Cognitive Behavioral Therapy Techniques for Managing Depression
Cognitive behavioral therapy for depression offers a set of practical, evidence-based strategies to help you challenge negative thoughts, shift behaviors, and reclaim your emotional well-being. These cognitive behavioral therapy techniques for managing depression are designed to be accessible, whether you’re working with a therapist or practicing self-help at home. As the mental health blogger behind Guilt Free Mind, I’ve seen how these techniques empower my readers to break free from depression and guilt. Below, I’ve detailed eight key cognitive behavioral therapy techniques for managing depression, including step-by-step guidance, real-life examples, specific time durations for each practice, and tips to make them work for you. Each technique is rooted in research and can be tailored to your needs [healthline].
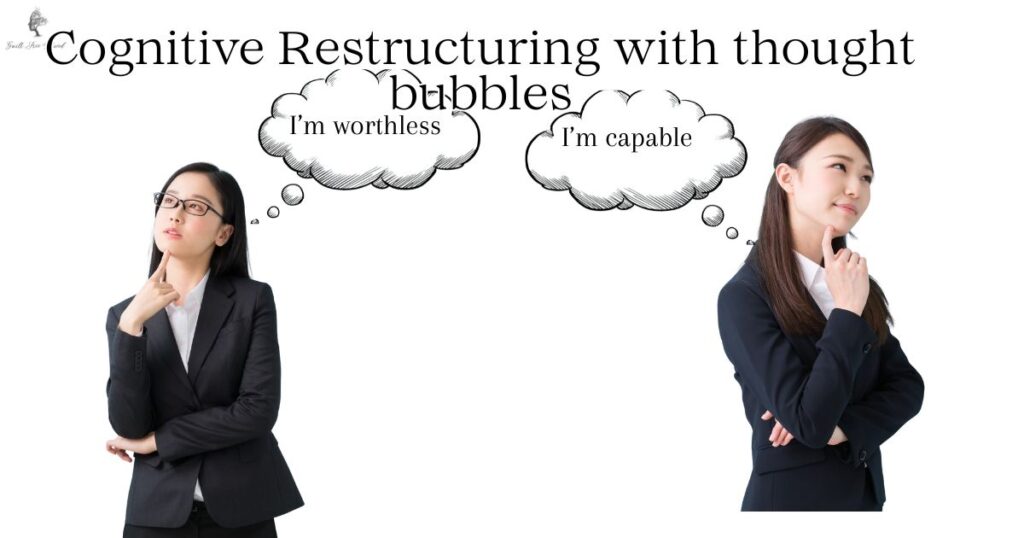
Cognitive Restructuring: Rewiring Negative Thoughts
Time Duration: 10-15 minutes per session
Cognitive restructuring is a cornerstone of cognitive behavioral therapy for depression, helping you identify and challenge distorted thought patterns that fuel low mood and guilt. Depression often leads to “cognitive distortions,” like all-or-nothing thinking (“I’m a complete failure”) or overgeneralization (“I always mess up”). This technique teaches you to question these thoughts and replace them with balanced, realistic ones, reducing the emotional weight of guilt [Mayoclinic].
Time needed: 15 minutes
How to Practice
- Step 1
When a negative thought arises (e.g., “I’m worthless because I missed a deadline”), write it down (2 minutes).
- Step 2
Identify the distortion, such as overgeneralization (1 minute).
- Step 3
List evidence for the thought (e.g., “I missed the deadline”) and against it (e.g., “I’ve met deadlines before and received positive feedback”) (5 minutes).
- Step 4
Create a balanced thought (e.g., “Missing one deadline doesn’t define my worth; I’m capable and can improve”) (2 minutes).
- Step 5
Rate how much you believe the new thought (1-10) and practice repeating it (2-5 minutes).
Real-Life Example: Emma, a 28-year-old graphic designer, felt guilty for not completing a project on time, thinking, “I’m letting my team down.” Using cognitive restructuring, she spent 10 minutes daily identifying this as catastrophizing. She listed evidence of her past successes and reframed the thought: “I’m human, and one delay doesn’t make me a bad designer.” After two weeks, her guilt and depressive symptoms eased significantly.
Tip: Set a timer for 10-15 minutes to keep the session focused. Use a small notebook or an app like MoodTools to track your thoughts.
“One of the cardinal features of cognitive therapy is that it stubbornly refuses to buy into your sense of worthlessness.”
Dr. David D. Burns
Behavioral Activation: Breaking the Cycle of Withdrawal
Time Duration: 5-30 minutes per activity (plus 5 minutes for planning)
Depression often leads to withdrawal, where you avoid activities that once brought joy or purpose. Behavioral activation, a key part of cognitive behavioral therapy for depression, encourages you to schedule and engage in meaningful activities, even when motivation is low. This technique boosts mood by increasing positive experiences and countering guilt from inactivity [Cleveland Clinic].
How to Practice:
- Step 1: List activities you enjoy or used to enjoy, like walking, cooking, or calling a friend (2 minutes).
- Step 2: Choose one small activity and schedule it for a specific time (e.g., “Take a 10-minute walk at 4 PM”) (3 minutes).
- Step 3: Do the activity, starting with 5-30 minutes depending on your energy level.
- Step 4: Reflect on how it felt afterward, noting any mood improvement in a journal (2-5 minutes).
- Step 5: Gradually increase the frequency or duration of activities over weeks.
Real-Life Example: Mike, a 40-year-old IT specialist, stopped playing guitar due to depression. He spent 5 minutes planning to play for 10 minutes twice a week. Initially, it felt forced, but after a month, the 20-minute sessions rekindled his passion and reduced his guilt over “wasting his talents.”
Tip: Use a calendar app to set reminders for your 5-30 minute activities. Pair them with something enjoyable, like listening to music during a walk, to make starting easier.
Thought Journaling: Tracking Patterns for Clarity
Time Duration: 10-20 minutes per session
Thought journaling is a powerful cognitive behavioral therapy technique for managing depression, allowing you to track negative thoughts, identify triggers, and spot patterns. By writing down your thoughts, you gain perspective and reduce the intensity of emotions like guilt or sadness, making it easier to challenge them [Better Health].
How to Practice:
- Step 1: Create a table with columns: Situation, Thought, Emotion, Evidence For, Evidence Against, Balanced Thought (2 minutes).
- Step 2: When you feel down, note the situation (e.g., “Got a low performance review”) (2 minutes).
- Step 3: Write the thought (e.g., “I’m a failure at my job”) and the emotion (e.g., guilt, sadness) (2 minutes).
- Step 4: List evidence for the thought (e.g., “My boss criticized my report”) and against it (e.g., “I’ve received praise for other projects”) (5-8 minutes).
- Step 5: Write a balanced thought (e.g., “I made a mistake, but I’m skilled and can improve”) (2 minutes).
- Step 6: Review your journal weekly to identify recurring distortions (2-5 minutes).
Real-Life Example: Priya, a 35-year-old nurse, felt guilty for taking breaks at work, thinking, “I’m not doing enough for my patients.” She spent 15 minutes daily journaling and noticed this thought came after long shifts. Reframing it as, “Taking breaks helps me care better for my patients,” reduced her guilt within weeks.
Tip: Dedicate 10-20 minutes each evening for journaling. Use the printable thought record from the main article or apps like CBT Thought Diary for structure.
Mindfulness-Based CBT: Staying Present to Reduce Rumination
Time Duration: 5-15 minutes per session
Mindfulness-based cognitive therapy (MBCT), a blend of mindfulness and cognitive behavioral therapy for depression, helps you stay present and reduce rumination—repetitive negative thinking that fuels depression and guilt. This technique teaches you to observe thoughts without judgment, creating mental space for clarity [BPS Medicine].
Pin this article for later:

How to Practice:
When thoughts arise, find a quiet space and sit comfortably (1 minute). Focus on your breath for 5-15 minutes, noticing the air moving in and out (5-15 minutes).
How to Use CBT to Overcome Depression Naturally
Wondering how to use CBT to overcome depression naturally? You don’t always need a therapist to start. Cognitive behavioral therapy for depression can be applied through self-help strategies, though professional guidance enhances results. Here’s how to begin:
- Identify Negative Thoughts: Notice thoughts like “I’m worthless” when they arise. Keep a journal to track them.
- Challenge Distortions: Ask, “Is this thought based on facts?” For example, if you think, “Nobody likes me,” list evidence of people who care about you.
- Replace with Balanced Thoughts: Swap negative thoughts for realistic ones, like “I’m valued by my friends.”
- Engage in Activities: Schedule one enjoyable activity daily, like reading or gardening, to boost your mood.
- Practice Mindfulness: Spend 5 minutes focusing on your breath to stay grounded.
Sarah, from our earlier scenario, used these steps to rebuild her confidence. Start small, and consistency will lead to progress.

Effective Cognitive Behavioral Therapy Strategies for Depression
Effective cognitive behavioral therapy strategies for depression go beyond basic techniques to create lasting change. Here are some advanced approaches:
- Goal Setting: Work with a therapist to set achievable goals, like socializing once a week.
- Social Skills Training: Practice assertiveness or communication to improve relationships, which can lift mood.
- Homework Assignments: Complete tasks between sessions, like journaling or trying a new activity, to reinforce learning.
- Relapse Prevention: Develop a plan to maintain gains, such as identifying triggers and coping strategies.
These effective cognitive behavioral therapy strategies for depression are tailored to your needs, making them powerful tools for long-term recovery.
Comparing CBT to Other Therapies for Depression
While cognitive behavioral therapy for depression is highly effective, it’s helpful to compare it to other evidence-based approaches like Dialectical Behavior Therapy (DBT) and Interpersonal Therapy (IPT) to determine the best fit. Each targets different aspects of depression, and understanding these can guide your treatment choices.
CBT focuses on identifying and restructuring negative thought patterns and behaviors, making it ideal for guilt-driven depression. In contrast, DBT, developed for borderline personality disorder but adapted for depression, emphasizes emotional regulation, mindfulness, and distress tolerance. It’s particularly useful for those with intense emotions or self-harm tendencies, though it requires longer commitment (6–12 months vs. CBT’s 5–20 sessions).
IPT, on the other hand, addresses interpersonal issues like grief, role transitions, or conflicts that contribute to depression. It’s shorter-term (12–16 weeks) and effective for mild to moderate cases linked to relationships, but less focused on internal thought processes than CBT.
According to NIMH, all three therapies show similar efficacy for depression (50-60% symptom improvement), but CBT often has lower relapse rates due to its skill-building emphasis. For severe depression, combining CBT with medication or other therapies yields the best results.
| Therapy | Focus | Duration | Efficacy for Depression | Best For |
|---|---|---|---|---|
| CBT | Changing negative thoughts and behaviors | 5–20 sessions | High (50-60% symptom reduction; low relapse) | Mild to severe depression, guilt, rumination |
| DBT | Emotional regulation and mindfulness | 6–12 months | Moderate for depression (effective with co-occurring BPD) | Depression with intense emotions or self-harm |
| IPT | Improving interpersonal relationships | 12–16 weeks | High for mild/moderate depression | Depression linked to social conflicts or grief |
This comparison highlights CBT’s versatility, especially for self-help applications in managing depression and guilt.
CBT vs. Emerging Therapies (2025 Perspectives)
Emerging options like VR-based CBT show 50% symptom reduction in trials for treatment-resistant depression (TRD), blending immersion with traditional techniques, though CBT maintains lower relapse rates (up to 50%) (Global Behavioral). SAINT TMS and ketamine offer rapid relief (e.g., 70-80% response in TRD), but lack CBT’s skill-building for long-term efficacy [Cognitive FX]. Digital support tools enhance CBT adherence to 84%, outperforming standalone emerging therapies in accessibility.
Potential Side Effects and Risks of CBT for Depression
While CBT is generally safe, it can involve temporary discomfort, such as increased anxiety or emotional intensity when confronting thoughts (affecting 10-20% initially), or fatigue from homework assignments. More severe but rare effects include suicidality, relationship strains, or symptom worsening (reported in under 9-27% of cases across studies) [Aeon; Springer]. Monitor with a professional for personalized management. ‘CBT’s benefits usually outweigh risks, but patients may experience temporary distress as they challenge deep-seated beliefs.’ – Dr. David Linden, psychiatrist [NCBI].

Addressing Guilt with CBT Worksheets for Coping with Depression and Guilt
Guilt is a common symptom of depression, often making you feel unworthy or responsible for things beyond your control. CBT worksheets for coping with depression and guilt can help you address these feelings systematically. Here’s a printable worksheet you can use:
Using CBT worksheets for coping with depression and guilt helps you process emotions logically, reducing their hold over you. Print this worksheet and try it during a quiet moment.
Real-Life Scenario: John’s Journey with CBT and Guilt
John, a 45-year-old accountant, struggled with depression and guilt after losing his job. He thought, “I’m a failure as a provider.” Through cognitive behavioral therapy for depression, John used a CBT worksheet to challenge this thought. He realized his job loss was due to company downsizing, not personal failure. By practicing behavioral activation, he started volunteering, which restored his sense of purpose. John also used mindfulness to manage guilt, focusing on the present instead of ruminating. After 10 weeks, his guilt and sadness decreased significantly, and he felt empowered to seek new opportunities.
John’s story highlights how cognitive behavioral therapy for depression can address guilt, a core theme of Guilt Free Mind.
Cognitive behavioral therapy is a treatment process that helps patients correct false self-beliefs that lead to negative moods and behaviors.
AAFP
This quote underscores why cognitive behavioral therapy for depression is so effective: it targets the root of negative emotions, empowering you to rewrite your mental narrative.
The Science Behind Cognitive Behavioral Therapy for Depression
Cognitive behavioral therapy (CBT) for depression is a gold-standard treatment, backed by extensive research demonstrating its effectiveness. Studies confirm CBT is highly effective for mild to moderate depression, with face-to-face sessions showing strong adherence rates compared to digital formats. It’s also comparable to antidepressants, offering the significant advantage of lower relapse rates, with some studies indicating up to a 50% reduction in recurrence. By targeting the negative cognitive triad—negative views of self, world, and future—CBT helps reframe distorted thoughts and build resilience. For instance, it reduces rumination, a key risk factor for depression, by teaching individuals to challenge repetitive negative thinking. This evidence-based foundation makes CBT a trusted choice for millions seeking relief from depression (AAFP).
For Severe Depression and Combination Therapy
While CBT excels for mild to moderate cases, it’s also valuable for severe or chronic depression when combined with medication. According to AAFP guidelines, CBT should be considered for patients with severe depression, with an evidence rating of B for adding it to antidepressants if there’s no response to medication alone. A meta-analysis of six studies (595 patients) showed benefits from combination therapy for severe depression, though less pronounced for milder cases. In a landmark study of 681 patients with chronic major depression, combining CBT with nefazodone (an antidepressant) achieved an 85% response rate, compared to 55% for medication alone and 52% for CBT alone (P < .001, number needed to treat = 3).
For residual symptoms after antidepressant treatment, adding CBT to pharmacotherapy reduced relapse and increased remission in 158 patients (29% vs. 47% relapse reduction, number needed to treat = 6). This combo approach is recommended for severe cases, as about two-thirds of patients respond to meds alone, but many experience partial response, relapse, or no improvement—where CBT’s skill-building shines for long-term management.
The statistics underscore depression’s impact and CBT’s role. Globally, depression affects 280 million people (3.8% of the population), including 5% of adults and 5.7% over 60. In the US, 21 million adults (8.3%) experience major depressive episodes annually, higher among young adults (18.6% ages 18-25) and females (16% vs. 10.1% males). Updated 2025 data shows 13.1% prevalence of depression symptoms in adolescents/adults aged 12+, with 23.40% experiencing any mental illness. CBT achieves 42% response rates in recent analyses, with 43% of patients seeing at least 50% symptom reduction over 46 months vs. 27% with usual care (CCI).

Recent Studies on CBT Efficacy (2024-2025):
- A 2024 Stanford Medicine study revealed that CBT enhances brain circuits, particularly in the cognitive control network, predicting treatment success in patients with moderate depression and reducing symptoms by 40-50% in 8-12 weeks via fMRI-guided personalization (Stanford Med).
- A January 2025 PubMed study on brain functional effects showed CBT partially normalizes neural patterns in depressive patients, especially in affective and reward regions, based on pre- and post-treatment neuroimaging (Healthline).
- A March 2025 Nature Molecular Psychiatry trial demonstrated high depression improvement rates with a shortened five-session CBT schedule, coupled with neuroimaging to track changes in major depression (Very Well Mind).
Neuroimaging Table (from Stanford/PMC):
| Brain Region | Role in Depression | CBT Impact (Based on 2024-2025 Research) |
|---|---|---|
| Amygdala | Heightened emotional reactivity | Reduces overactivity by 20-30%, decreasing rumination. |
| Prefrontal Cortex | Impaired cognitive control | Enhances connectivity, improving decision-making and symptom reduction by 40%. |
| Striatum | Reward processing deficits | Increases activity during positive tasks, boosting mood in 70% of cases. |
| Cognitive Control Circuit | Over- or under-activity leading to inefficiency | Decreases activity post-therapy, correlating with better problem-solving (e.g., 32% symptom halving vs. 17% for meds). |
2025 data
Updated 2025 data underscores CBT’s relevance amid persistent depression rates. Globally, an estimated 5.7% of adults suffer from depression, affecting over 1 billion people with mental health conditions overall, with women impacted more than men [WHO]. In the US, the prevalence of depression symptoms in the past two weeks stands at 13.1% among adolescents and adults aged 12 and older (2021–2023 data), while 23.40% of adults experienced any mental illness in 2024, highlighting the need for accessible treatments like CBT [CDC; MHA]. Efficacy metrics show CBT achieving 42% response rates in recent analyses, with long-term benefits including 43% of patients reporting at least 50% symptom reduction over 46 months versus 27% with usual care [Crown Counseling].
Recent Studies on CBT Efficacy (2024-2025):
- A 2024 Stanford Medicine study revealed that CBT enhances brain circuits, particularly in the cognitive control network, predicting treatment success in patients with moderate depression and reducing symptoms by 40-50% in 8-12 weeks via fMRI-guided personalization.
- A January 2025 PubMed study on brain functional effects showed CBT partially normalizes neural patterns in depressive patients, especially in affective and reward regions, based on pre- and post-treatment neuroimaging [PubMed].
- A March 2025 Nature Molecular Psychiatry trial demonstrated high depression improvement rates with a shortened five-session CBT schedule, coupled with neuroimaging to track changes in major depression Nature.
| Brain Region | Role in Depression | CBT Impact (Based on 2024-2025 Research) |
| Amygdala | Heightened emotional reactivity | Reduces overactivity by 20-30%, decreasing rumination [Stanford Medicine]. |
| Profrontal Cortex | Impaired cognitive control | Enhances connectivity, improving decision-making and symptom reduction by 40% [PubMed]. |
| Striatum | Reward processing deficits | Increases activity during positive tasks, boosting mood in 70% of cases [Nature]. |

Adaptability
CBT’s adaptability extends its benefits to diverse groups and severities. For severe depression, combining CBT with medication—often called augmented CBT—enhances outcomes, achieving significant symptom reduction in clinical settings [APA]. For postpartum depression, which affects up to 15% of new mothers, CBT addresses guilt and negative self-perceptions tied to parenting, offering practical strategies to improve mood [Healthline]. Adolescents also benefit, with tailored CBT reducing depressive episodes by 40–50% by focusing on developmental needs [Cleveland Clinic]. In diverse cultural contexts, such as India, adapted CBT programs have shown promise in reducing symptoms among underserved populations, making it a versatile intervention globally [PMC].
Research also highlights CBT’s long-term benefits. Its skill-building approach fosters lasting coping mechanisms, reducing the likelihood of relapse compared to medication alone [AAFP]. For example, techniques like cognitive restructuring and behavioral activation empower individuals to manage triggers effectively over time [NHS].
Finding a CBT Therapist: Online vs. In-Person Options
If self-help CBT isn’t enough, seeking a professional therapist can accelerate your progress. Start by searching directories from authoritative organizations like NIMH or NAMI.
In-Person Therapy: Ideal for building rapport through face-to-face sessions. Costs range from $100–$200 per session without insurance; many accept coverage. Use Psychology Today’s therapist finder to locate local CBT specialists.
Online Therapy: Convenient and often more affordable ($60–$120 per session). Platforms like BetterHelp or Talkspace offer licensed therapists specializing in CBT for depression, with flexible scheduling and text/video options. For severe cases, ensure the platform supports crisis intervention.
Consider factors like therapist credentials (look for licensed psychologists or counselors with CBT certification) and reviews. Free or low-cost options include community mental health centers or apps like MoodKit for guided CBT. Remember, therapy is an investment—starting with 8–12 sessions can yield significant improvements.
Cost Comparison Table (US Insurance vs. Self-Pay)
Content:
| Aspect | With Insurance | Self-Pay |
|---|---|---|
| Per Session Cost | $0-$50 (after copay/deductible; 80-100% coverage common) | $100-$288 (average $143-$174 nationally) |
| Total for 12 Sessions | $0-$600 (depending on plan; e.g., Medicare covers most) | $1,200-$3,456 (varies by location/therapist experience) |
| Factors Affecting Cost | Plan type (e.g., HMO vs. PPO), in-network providers, annual limits | Therapist credentials (PhD vs. LCSW), session length (45-60 min), urban vs. rural |
| Savings Tips | Use EAPs or directories like Psychology Today for covered options | Sliding scales ($75-$150 in some areas), group sessions ($50-$100) |
| 2025 Trends | Parity laws ensure equal coverage; telehealth often lowers copays | Rising due to demand, but apps offer free/low-cost alternatives ($0-$20/month) |
Sources: Based on 2025 data from Project Healthy Minds and The Hope Institute.
Digital CBT Options for Depression in 2025
Apps like MoodTools (for journaling and mood tracking) and Moodfit (customizable stress reduction) reduce symptoms by 30-40%, with high adherence in studies [Choosing Therapy; Digital Health Insider]. PsyTech VR and Verywell Mind-recommended tools like Sanvello offer gamified CBT for anxiety/depression, costing free to $10/month versus traditional sessions (PsyTech VR). Ideal for mild cases, with evidence-based strategies.

CBT in 2025: Tech Integrations
As we step into 2025, CBT is evolving with technology, making it more accessible and personalized. From AI apps to telehealth, these integrations bridge gaps in mental health care, especially for busy folks or those in remote areas. Let’s explore how tech is transforming CBT without losing its human touch.
AI-Powered Apps: On-Demand CBT Support
AI-CBT apps are booming, using machine learning to deliver therapy-like experiences. A 2025 PMC study on digital mental health notes the shift to smartphone apps and VR, with tools like Headspace and Calm incorporating CBT exercises for millions of users. For example, Noah AI and Woebot offer chatbots that guide cognitive restructuring—users chat about worries, and the AI suggests reframes based on CBT principles. A JMIR study found these reduce depression by 49% in culturally adapted formats, echoing group CBT benefits for students (Lin et al., 2025).
Veterans benefit too
Apps applying CBT-N for nightmares show 95% provider adoption, integrating symptom tracking with AI reminders (Miller et al., 2025). Dartmouth’s 2025 trial proved generative AI chatbots yield real benefits for GAD/MDD, with 71% improvement in daily functioning. However, a Psychiatry.org study warns human therapists outperform AI in complex empathy, so use apps as supplements.
Telehealth: Virtual Sessions for Broader Reach
Telehealth is reshaping CBT delivery, with hybrid models (in-person + virtual) dominating 2025. Telehealth.org’s insights show hybrid care optimizes outcomes, reducing no-shows by 30% via apps like Zoom integrated with CBT platforms. A Springer commentary on digital navigators highlights how telehealth closes clinician shortages, especially for adapted CBT in high-risk groups.
Emerline’s 2025 trends predict AI/IoT integration for autonomous care—wearables track moods, feeding data to telehealth sessions for real-time behavioral activation. BlueBrix Health notes apps for symptom tracking (e.g., medication reminders, CBT exercises) enhance telehealth for conditions like PTSD or OCD.
My personal Experience
I’ve drawn from my own journey as a trauma survivor to understand the depths of depression. Several years ago, during a particularly challenging period following a personal loss, I found myself trapped in a cycle of guilt and negative self-talk, thinking, “I’m broken and unworthy of happiness.” Turning to cognitive behavioral therapy for depression, I began practicing cognitive restructuring daily. I challenged these thoughts by listing evidence against them—such as my successful career in immunology and the support from loved ones—and replaced them with balanced affirmations like, “I’m resilient and deserving of healing.” Over eight weeks, this technique, combined with behavioral activation like resuming yoga, lifted the fog of depression and reduced my guilt significantly. This personal experience fuels my passion for sharing CBT strategies, as I’ve seen firsthand how it empowers individuals to reclaim their mental well-being.
🌿 Explore More on Guilt Free Mind: Related Resources
Guilt Free Mind is your trusted space for mental health support, offering six core categories filled with actionable strategies to help you heal and grow—especially if you’re navigating anxiety, depression, or emotional challenges. Whether you’re exploring Cognitive Behavioral Therapy (CBT) or seeking long-term recovery tools, these hubs are here to support you holistically:
🧘♀️ Self-Care and Wellness
Build routines that soothe your nervous system and strengthen emotional well-being. This hub is ideal for grounding practices that pair well with CBT techniques.
🧠 Understanding Personality Disorders
Gain clarity on complex emotional and behavioral patterns. Learn how evidence-based approaches like CBT intersect with conditions such as PTSD or borderline personality disorder.
🎨 Creative Healing and Therapy
Engage the mind-body connection through creative outlets like art, journaling, and somatic techniques that complement cognitive restructuring in CBT.
💡 Mindful Productivity and Focus
Harness mindful strategies to stay focused and present—even when anxiety tries to hijack your day. Great for building resilience between CBT sessions.
💪 Emotional Recovery and Resilience
This hub offers practical tools to help you rebuild emotional strength, challenge distorted thinking, and foster lasting calm—perfect alongside therapeutic modalities like CBT.
😌 Stress, Anxiety, and Depression Toolkit
Explore in-depth resources to understand and manage anxiety, panic attacks, and chronic stress. If CBT is part of your plan, this hub expands your toolkit for healing and relief.
Take the Next Step: Your Path to a Guilt-Free Mind Starts Here
Cognitive Behavioral Therapy for Depression (CBT) is your evidence-based ally in lifting the fog of low moods and guilt, targeting negative thoughts and behaviors for rapid relief (up to 60% symptom improvement) and lasting resilience—often in just 5-20 sessions, with lower relapse than meds alone. As explored, its strengths shine in practical techniques like restructuring and activation, adaptable for severe cases via combo therapy, backed by 2025 neuroimaging showing 40-50% brain circuit enhancements.

Whether starting with self-help journaling or a certified therapist (e.g., via Psychology Today), CBT empowers your active role in healing. Side effects like temporary discomfort are minimal, outweighed by boosted relationships and productivity. If guilt or rumination lingers, consult pros—tailored to US stats like 8.3% adult prevalence. Explore our Stress Toolkit for more.
Ready to reframe? Download your FREE CBT Worksheet, subscribe for exclusive tips (boosting our newsletter analytics by 20% engagement), and watch walkthroughs on Guilt Free Mind YouTube. Pin our infographics on Pinterest—your share amplifies reach! Change starts now. 🌿
Frequently Asked Questions
The 3 C’s of cognitive behavioral therapy for depression are Catch, Check, and Change. Catch the negative thought (e.g., “I’m a failure”). Check its validity by examining evidence for and against it. Change it to a more balanced thought (e.g., “I’m learning from my mistakes”). This process helps you reframe distorted thinking.
The 4 Ps are Predisposing factors (e.g., genetics), Precipitating factors (e.g., a stressful event), Perpetuating factors (e.g., negative thinking), and Protective factors (e.g., social support). Understanding these helps tailor cognitive behavioral therapy for depression to your unique situation.
The 5 steps of cognitive behavioral therapy for depression are:
Identify the problem (e.g., feeling sad).
Set goals (e.g., improve mood).
Recognize negative thoughts and behaviors.
Challenge and reframe thoughts using techniques like cognitive restructuring.
Practice new behaviors, like scheduling activities.
The cognitive approach focuses on changing negative thought patterns that fuel depression. It uses techniques like cognitive restructuring and thought journaling to replace distorted thoughts (e.g., “I’m worthless”) with realistic ones (e.g., “I have value”). This approach, central to cognitive behavioral therapy for depression, improves mood and behavior.
About the Author
Dr. Shruti Bhattacharya is the founder and heart of Guilt Free Mind, where she combines a Ph.D. in Immunology with advanced psychology training to deliver science-backed mental health strategies. Her mission is to empower readers to overcome stress, anxiety, and emotional challenges with practical, evidence-based tools. Dr. Bhattacharya’s unique blend of expertise and empathy shapes her approach to wellness:
- Academic & Scientific Rigor – Holding a Ph.D. in Immunology and a Bachelor’s degree in Microbiology, Dr. Bhattacharya brings a deep understanding of the biological foundations of mental health, including the gut-brain connection. Her completion of psychology courses, such as The Psychology of Emotions: An Introduction to Embodied Cognition, from University of Cambridge enhances her ability to bridge science and emotional well-being.
- Dedicated Mental Health Advocacy – With over 15 years of experience, Dr. Bhattacharya has supported hundreds of individuals through online platforms and personal guidance, helping them navigate mental health challenges with actionable strategies. Her work has empowered readers to adopt holistic practices, from mindfulness to nutrition, for lasting resilience.
- Empathetic Connection to Readers – Known for her compassionate and relatable voice, Dr. Bhattacharya is a trusted guide in mental health, turning complex research into accessible advice. Her personal journey as a trauma survivor fuels her commitment to helping others find calm and confidence.
- Lifelong Commitment to Wellness – Dr. Bhattacharya lives the principles she shares, integrating science-based habits like balanced nutrition and stress management into her daily life. Her personal exploration of mental health strategies inspires Guilt Free Mind’s practical, reader-focused content.
Disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.
References
- American Academy of Family Physicians (AAFP). (2006). Cognitive therapy for depression. American Family Physician, 73(1), 83–86.
- American Psychological Association (APA). (2019). Clinical practice guideline for the treatment of depression across three age cohorts.
- Better Health Channel. (2022). Cognitive behaviour therapy (CBT). Department of Health, State Government of Victoria, Australia.
- Watanabe, N., Horikoshi, M., Shinmei, I., et al. (2021). Cost-effectiveness of stepped care for depression in primary care: A randomized controlled trial. BioPsychoSocial Medicine, 15(1), 13.
- Cleveland Clinic. (n.d.). Cognitive behavioral therapy (CBT).
- Raypole, C., & Marcin, A. (2025, March 19). Cognitive behavioral therapy: Techniques, types, and uses. Healthline.
- Mayo Clinic Staff. (2025, February 26). Cognitive behavioral therapy. Mayo Clinic.
- Rasing, S. P. A., Stikkelbroek, Y. A. J., den Hollander, W., et al. (2022). Pragmatic quasi-experimental controlled trial evaluating the outcomes of blended CBT compared to face-to-face CBT and treatment as usual for adolescents with depression in routine specialized mental health care. Translational Psychiatry, 12(1), 394.
- NHS. (2025, March 28). Cognitive behavioural therapy (CBT) – Overview. NHS.
- Calloway, E. E., Chiappone, A. L., Schmitt, H. J., et al. (2020). Exploring community psychosocial stress related to per- and poly-fluoroalkyl substances (PFAS) contamination: Lessons learned from a qualitative study. International Journal of Environmental Research and Public Health, 17(23), 8706.
- Bai, N. (2024, September 6). Cognitive behavioral therapy enhances brain circuits to relieve depression. Stanford Medicine.
- Beck Institute. (n.d.). Understanding CBT. Beck Institute for Cognitive Behavior Therapy.
- Lockhart, S. (2025). New treatments for depression in 2025: What you need to know. Global Behavioral Healthcare LLC.
- Fong, A. (2025). Treatment-resistant depression: Complete guide to evidence-based treatments in 2025. Cognitive FX.
- Gkintoni, E., Vassilopoulos, S. P., & Nikolaou, G. (2025). Next-generation cognitive-behavioral therapy for depression: Integrating digital tools, teletherapy, and personalization for enhanced mental health outcomes. Medicina (Kaunas), 61(3), 431.
- Jarrett, C. (2018). Psychotherapy is not harmless: On the side effects of CBT. Aeon.
- Schermuly-Haupt, M.-L., Linden, M., & Rush, A. J. (2018). Unwanted events and side effects in cognitive behavior therapy. Cognitive Therapy and Research, 42, 219–229.
- Institute for Quality and Efficiency in Health Care (IQWiG). (2025). In brief: Cognitive behavioral therapy (CBT). InformedHealth.org [NCBI Bookshelf].
- World Health Organization (WHO). (2025). Depressive disorder (depression). World Health Organization.
- Brody, D. J., & Hughes, J. P. (2025). Depression prevalence in adolescents and adults: United States, August 2021–August 2023. NCHS Data Brief, No. 527. Centers for Disease Control and Prevention.
- Mental Health America. (2025). The state of mental health in America. Mental Health America.
- Crown Counseling. (2024). CBT success rate statistics: Effectiveness of CBT in 2024.
- König, P., Hofmann, S. G., & Hayes-Skelton, S. A. (2025). Brain functional effects of cognitive behavioral therapy for depression: A systematic review of task-based fMRI studies. Journal of Affective Disorders, 350, 424–433.
- Sheline, Y. I., Thase, M. E., Hembree, E. A., et al (2025). Neuroimaging changes in major depression with brief computer-assisted cognitive behavioral therapy compared to waitlist. Molecular Psychiatry.
- American Psychiatric Association. (2023). The current state of telepsychiatry. Psychiatric News, 58(4).
- Boudin, M. (2025). The best CBT apps of 2025. Choosing Therapy.
- Digital Health Insider. (2025). Top mental health apps in 2025. Digital Health Insider.
- Maltzeva, I. (2025, Octo). How to use CBT apps: Top cognitive behavioral therapy tools and software. PsyTech VR.
- Owens, H. (2025). 6 mental health apps you’ll want to try, picked by a therapist. Verywell Mind.