Last Updated On: December 13th, 2025
Hey there, if you’re checking this out, you’re probably one of my readers looking for solid ways to tackle mental health hurdles. I’ve connected with so many who feel bogged down by persistent worries or down moods, and cognitive behavioral therapy (CBT) has proven to be a real shift for them. As a mental health blogger, I draw from reliable sources to explain how CBT can help reframe those tricky thought patterns into something more manageable. Cognitive behavioral therapy connects thoughts, feelings, and behaviors, giving you actionable ways to make changes.
This guide dives deep into cognitive behavioral therapy, from its background to real-world uses, supported by studies and stories. We’ll touch on how does CBT work for anxiety, CBT techniques for depression at home, and other specifics. With examples, data, and tips, it’s designed to help you apply it right away.

Table of Contents
At a Glance: Cognitive Behavioral Therapy (CBT)
| Key Aspect | Details |
|---|---|
| What is CBT? | A structured, goal-oriented therapy focusing on changing negative thought patterns and behaviors to improve mental health (PMC, 2020). |
| Best For | Anxiety disorders (e.g., GAD, social anxiety, panic), depression, OCD, PTSD; effective as standalone or add-on to meds. |
| Core Techniques | Cognitive restructuring, exposure therapy, behavioral activation, thought records, relaxation training. |
| Duration & Sessions | Typically 5-20 sessions, 45-60 minutes each; short-term with homework for self-practice. |
| Benefits | Rapid symptom reduction (50-80% improvement), lasting relief, lower relapse than meds alone, builds lifelong skills. |
| Evidence | Backed by meta-analyses, large effect sizes (0.5-1.75) for anxiety/trauma; first-line in US guidelines (NIMH/APA). Backed by meta-analyses, large effect sizes (0.5-1.75) for anxiety/trauma; first-line in US guidelines (NIMH/APA); recent trials show adapted CBT reduces psychosis risk alongside depression/anxiety symptoms (Newman-Taylor et al., 2025). |
| Potential Drawbacks | Temporary discomfort from exposures; requires commitment to homework; not ideal for severe crises alone. |
| Cost & Access | Often covered by US insurance; find via ABCT.org; online options available for self-help. |
What is Cognitive Behavioral Therapy?
Cognitive behavioral therapy is a structured psychotherapy that targets the links between thoughts, emotions, and behaviors to ease mental health issues (Mayo Clinic, 2023). It helps spot negative thought patterns and swap them with balanced ones using methods like cognitive restructuring. Different from therapies that explore the past extensively, CBT is present-focused and short-term, usually 5-20 sessions, ideal for anxiety, depression, and beyond.
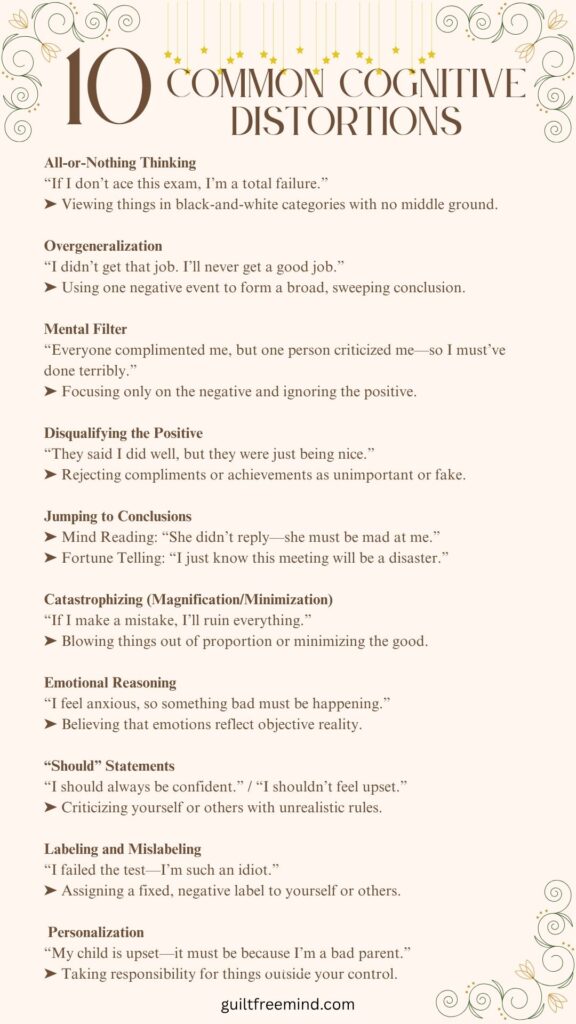
Central to it are automatic thoughts—those fast ideas that pop up and affect how we feel—and cognitive distortions, like jumping to conclusions. In therapist-guided sessions, you might use thought records for journaling to log and question these. As evidence-based therapy, it’s widely backed for mental health treatment.
A survey by the American Psychological Association shows cognitive behavioral therapy’s flexibility, blending in mindfulness and CBT for better emotional regulation (APA, 2023). For DIY approaches, use CBT worksheets to support home practice.
Case Study: Overcoming Catastrophizing with CBT
Meet Sarah (name changed for privacy), one of my readers who struggled with ongoing worry and generalized anxiety. She often fell into catastrophizing patterns, where minor setbacks spiraled into overwhelming fears—for instance, thinking, “This one mistake at work ruins my entire career and everything I’ve built.” Through applying Cognitive Behavioral Therapy (CBT) techniques learned from my resources, Sarah began identifying these distorted thoughts by journaling her triggers and evidence. She reframed them with balanced, fact-based perspectives, such as, “This is just a single error; I’ve had many successes before, and I can learn from it to improve.” Over a few weeks of consistent practice, including challenging her assumptions during daily routines, Sarah noticed a significant boost in her confidence and daily life—reducing rumination, improving sleep, and allowing her to handle challenges more resiliently. This real-world application highlights how CBT’s structured approach can transform anxiety into actionable growth.
Cognitive behavioral therapy (CBT) is a structured, goal-oriented type of talk therapy.”
Expert quote from the Cleveland Clinic
History of Cognitive Behavioral Therapy
The history of cognitive behavioral therapy traces to the mid-20th century, blending behaviorism and cognitive insights, with key origins in the works of Albert Ellis and Aaron Beck. Ellis developed Rational Emotive Behavior Therapy (REBT) in the 1950s, first announced in 1956, drawing from Alfred Adler and Abraham (National Center for Biotechnology Information, 2015). Low REBT stressed how irrational beliefs cause emotional distress, challenging them through rational analysis. Ellis’s 1962 book “Reason and Emotion in Psychotherapy” marked a milestone, outlining REBT’s focus on disputing unhelpful thoughts.
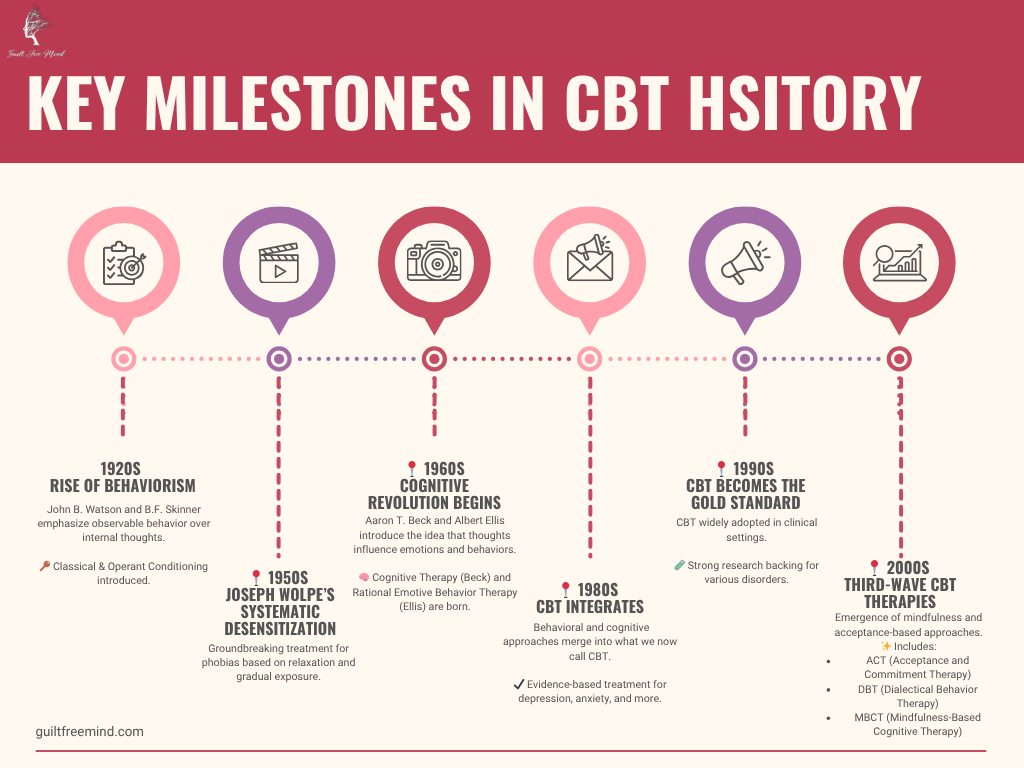
Aaron Beck, shifting from psychoanalysis in the late 1950s, noticed patients’ thoughts weren’t as unconscious as Freud claimed. This led to cognitive therapy, detailed in his 1967 publication, with the first treatment manual for depression in 1979. Beck, called the father of cognitive behavioral therapy, noted: “The philosophical origins of cognitive therapy can be traced back to the Stoic philosophers.” (Wiki) His cognitive model emphasized the triad of negative views on self, world, and future.
Roots in Behaviourism/ First Wave
Roots in behaviorism include early 20th-century work by John B. Watson and Rosalie Rayner on conditioning (1920), Mary Cover Jones on unlearning fears (1924), and Joseph Wolpe’s systematic desensitization (1950s), based on Pavlov. B.F. Skinner’s operant conditioning and Bandura’s social learning theory (1969) added layers. This “first wave” focused on behaviors.
Second Wave
The “second wave” in the 1960s-1970s integrated cognition as behaviorism waned during the cognitive revolution, with Ellis and Beck leading. By the 1980s-1990s, mergers formed modern cognitive behavioral therapy, like treatments for panic by Clark and Barlow. The “third wave” brought mindfulness, including Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT), as Hayes noted: “Third-wave CBT expands traditional methods by emphasizing contextual and experiential processes.” (NIH)
Philosophical ties include Stoicism (Epictetus) and Buddhism, influencing DBT and mindfulness-based cognitive therapy. Milestones: 1977 trial showing cognitive therapy beat medication for depression; over 2000 trials validate it today. (PMC) Cognitive behavioral therapy evolved into a versatile, evidence-based powerhouse.
CBT for Beginners: Your First Steps
CBT is like a mental workout: It trains you to spot unhelpful thoughts and replace them with balanced ones. Start with basics: Identify a “hot thought” (e.g., “I’m a failure because I messed up once”) and question it with evidence (e.g., “What successes have I had?”). Use free tools like our Thought Record Worksheet to log daily.
How Does Cognitive Behavioral Therapy Work for Anxiety?
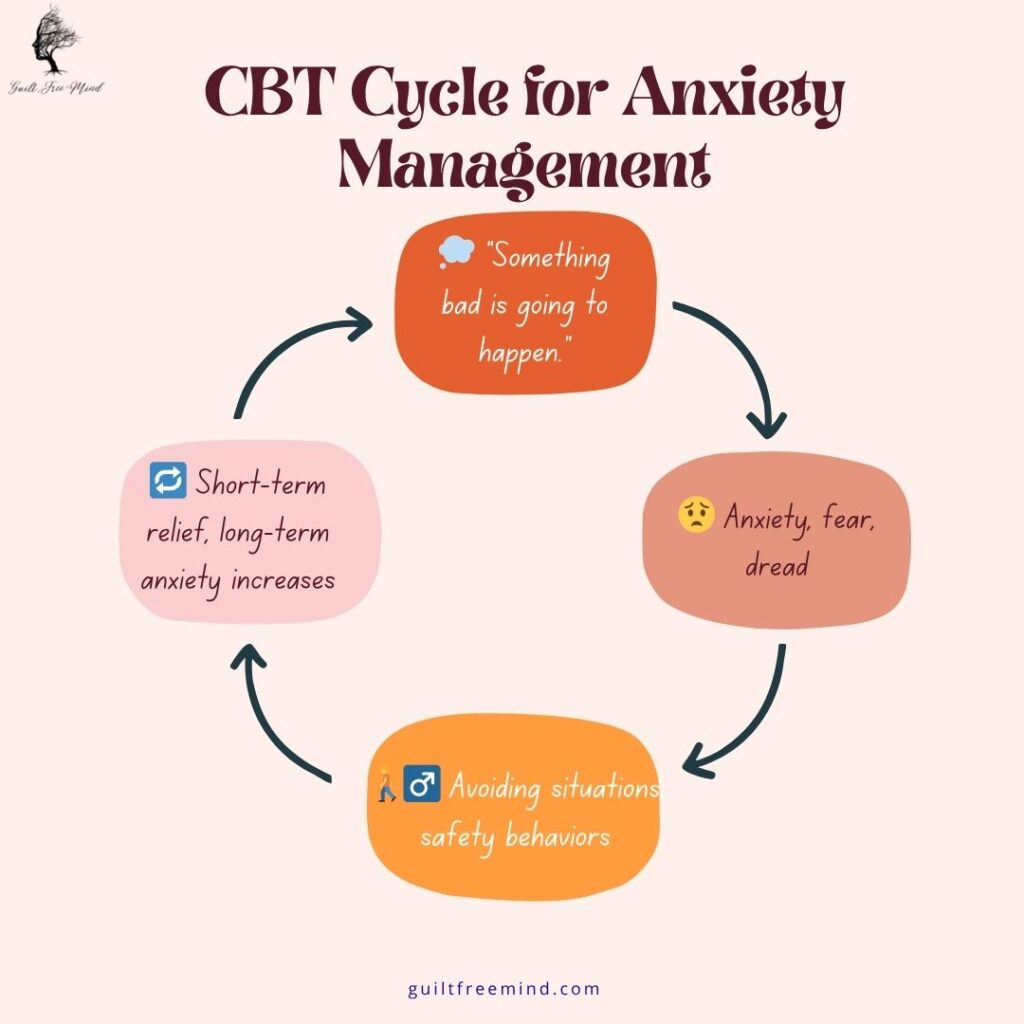
Cognitive behavioral therapy addresses anxiety by disrupting the thought-anxiety loop. It involves spotting automatic thoughts, then cognitive restructuring to test their truth (OCD UK 2023). Exposure therapy builds resilience by facing fears step-by-step.
Meta-analyses show cognitive behavioral therapy reduces anxiety symptoms by 50-60%, with remission rates around 51% across disorders (DIV). Adapted versions for high-risk populations, such as those with psychosis vulnerability, further signal sustained improvements in anxiety and relational factors over 3-12 months. A study found 71% reduced worry with app-based cognitive behavioral therapy. (Big Health)
“CBT for anxiety is more than just talking; it is like working with a personal trainer.”
– Therapist Emily Johnston:
In an interview, David Burns shared: “Cognitive therapy helps by showing distortions aren’t reality.” (Clear Thinking Podcast)
Case Study: Long-Term Benefits of Imaginal Exposure in GAD Treatment
In a landmark study reviewing CBT approaches, patients with Generalized Anxiety Disorder (GAD) who incorporated imaginal exposure—vividly imagining and recounting their worst-case worry scenarios to desensitize emotional responses—demonstrated superior long-term results compared to relaxation training alone. For instance, participants in protocols like those tested by Borkovec and Costello (1993) engaged in repeated self-guided imaginal sessions over 10 weeks, focusing on worries about health, relationships, or finances, which helped reduce the intensity of chronic rumination and physical symptoms like restlessness and muscle tension. At the 12-month follow-up, these individuals reported greater overall functioning, with fewer anxiety relapses and improved daily resilience, outperforming those relying solely on applied relaxation techniques, as meta-analyses confirmed CBT’s edge in sustained worry reduction without specific demographics highlighted.
Cognitive Behavioral Therapy Techniques for Depression: Practical Self-Help Strategies
For depression, CBT achieves response rates of approximately 49.5%, with meta-analyses showing large effect sizes (0.5–1.0) for symptom reduction (National Center for Biotechnology Information, 2018). Controlled trials in primary care settings confirm adapted CBT and higher recovery rates for depression/anxiety in at-risk groups. Group-based adaptations, such as incorporating cultural idioms, show sustained relief in depressive symptoms and sleep disturbances at 3-month follow-ups compared to standard CBT (Lin et al., 2025). Home-based cognitive behavioral therapy techniques help combat depression’s inertia. Behavioral activation means planning activities, like short walks, to spark momentum. Thought records involve noting situations, thoughts, and counter-evidence.
Meta-analyses indicate response rates of 49.5% for depression (Science Direct).
Expert quote from Simon Rego, PsyD: “There is a massive tidal wave of evidence for cognitive behavioral therapy that suggests it is very effective at treating certain problems” (Healthline, 2023). From David Burns podcast: “Feeling good comes from challenging those automatic negative thoughts” (Psych Central).
Case Study: Integrating ACT into CBT for GAD During a Pandemic
Fred, a 28-year-old graduate student, sought help for lifelong anxiety intensified by a recent breakup, presenting with excessive worry, restlessness, muscle tension, and sleep issues that disrupted his relationships and academics. Over 29 sessions spanning 10 months—shifting from in-person to virtual due to COVID-19—he followed a manualized CBT program (Mastery of Your Anxiety and Worry) enhanced with Acceptance and Commitment Therapy (ACT) elements, including psychoeducation, self-monitoring via worry records, progressive muscle relaxation, cognitive restructuring to challenge catastrophic thoughts, imaginal exposure to fears, mindfulness for present-moment awareness, cognitive defusion (e.g., labeling thoughts as “I’m having the thought that…”), and values clarification to align actions with personal goals.
Despite challenges like transitioning to telehealth and initial resistance to acceptance techniques, Fred achieved significant symptom relief: his GAD-7 score dropped from 11 (moderate) to 2 (minimal), PHQ-9 from 9 to 0, and reliable change indices showed marked improvements in anxiety (RCI=5.20), depression, and stress, with gains maintained at one-month follow-up through flexible strategy use (PMC)
Quick-Start Checklist for Home CBT:
- Spot one negative thought each day.
- Write evidence for and against it.
- Craft a balanced alternative.
- Do one mood-boosting activity.
- Track progress in a journal.

Benefits of Cognitive Behavioral Therapy for Social Anxiety Disorder: Lasting Relief and Skill-Building
Social Anxiety Disorder (SAD) often leads to intense fear of social situations, resulting in avoidance that can severely impact daily life, relationships, and opportunities. Cognitive Behavioral Therapy (CBT) addresses this by focusing on exposure techniques and cognitive restructuring, helping individuals confront fears head-on while reframing negative thoughts (Psychiatry Online, 2020). This structured approach boosts social confidence by gradually reducing avoidance behaviors, leading to lasting improvements in how people interact with the world.
Key Benefits of CBT for Social Anxiety
Rapid Symptom Reduction
CBT often delivers noticeable relief in 12-16 sessions, with reductions in anxiety symptoms, physical reactions like blushing or palpitations, and avoidance tendencies. Meta-analyses show CBT’s superiority over wait-list controls or relaxation therapies, with effect sizes indicating strong outcomes for both exposure and cognitive components.
Lasting Relief and Improved Functioning
Long-term follow-ups at 12 months reveal sustained benefits, including fewer relapses and enhanced social resilience, outperforming nondirective therapies. Patients report better overall functioning in social settings, such as improved performance at work or school.
Stronger Relationships and Quality of Life
By challenging catastrophic beliefs (e.g., “Everyone will reject me if I make a mistake”), and working on perfectionism, CBT fosters more authentic connections and a fuller life, reducing isolation and building interpersonal skills.
Skill-Building for Independence
Tools like thought records and hierarchical exposure empower self-management. For instance, initial exercises might involve recording conversations to check for perceived errors, progressing to “social cost” tasks like intentional public embarrassment to prove tolerability.
In the United States, social anxiety disorder affects about 7% of adults annually, contributing to the broader 19.1% past-year prevalence of any anxiety disorder.nimh.nih.gov CBT offers rapid relief, with studies showing 50-80% improvement rates in social functioning after 12-16 sessions. For instance, NIMH research indicates higher rates among younger adults (22.3% for ages 18-29), where CBT’s skill-building can prevent long-term isolation.
Expert Insight: “Exposure techniques rely on learning theory to explain how prolonged fear is maintained over time… [they] encourage a patient to confront a feared situation without engaging in avoidance or subtle safety behaviors,” which facilitates “new experiences of safety” and breaks the avoidance cycle in SAD (Psychiatry Online).
Cognitive Behavioral Therapy vs Medication for Panic Attacks: Weighing Options for Effective Management
When dealing with panic attacks, choosing between Cognitive Behavioral Therapy (CBT), medication, or other approaches involves considering factors like speed of relief, long-term sustainability, and potential risks. CBT emphasizes skill-building through exposure and cognitive tools to manage symptoms, while medication offers quick chemical intervention but may not address root causes. Psychoanalysis, on the other hand, delves into unconscious patterns for deeper insights. Understanding these options helps tailor treatment to individual needs, often combining methods for optimal results.
CBT vs. Medication vs. Psychoanalysis
| Therapy/Treatment | Duration | Focus | Effectiveness | Side Effects |
|---|---|---|---|---|
| CBT | Short (8-12 weeks) | Thoughts and behaviors, with exposure to build skills | Equals meds in symptom reduction (e.g., 50% improvement), lower relapse rates; strong for panic via interoceptive exposure.my.clevelandclinic.org | Minimal, though temporary discomfort from facing fears. |
| Medication (e.g., SSRIs or Benzodiazepines) | Ongoing | Symptom relief via brain chemistry | Quick onset but high relapse upon discontinuation; effective short-term but less for root causes.my.clevelandclinic.org | Drowsiness, dependency, withdrawal risks. |
| Psychoanalysis | Long (years) | Unconscious conflicts and past experiences | Deeper insights for some, longer-lasting in complex cases; less empirical data for panic.my.clevelandclinic.org | Emotional intensity, potential for prolonged distress without quick relief. |
CBT is also effective in helping manage nonpsychological medical conditions, highlighting its versatility beyond panic to broader anxiety management
Cleveland Clinic
One of my readers, John who was experiencing frequent panic attacks, blended CBT’s exposure techniques (e.g., inducing sensations like dizziness to desensitize) with short-term medication for initial control, achieving sustained management without long-term dependency (Harvard Health, 2024).
In US populations, panic disorder impacts about 2.7% of adults annually, with higher rates among females (23.4% overall anxiety prevalence vs. 14.3% for males). CBT matches medication in effectiveness (e.g., 50% symptom reduction) but shows lower relapse, per NIH meta-analyses, making it a first-line recommendation in US guidelines.
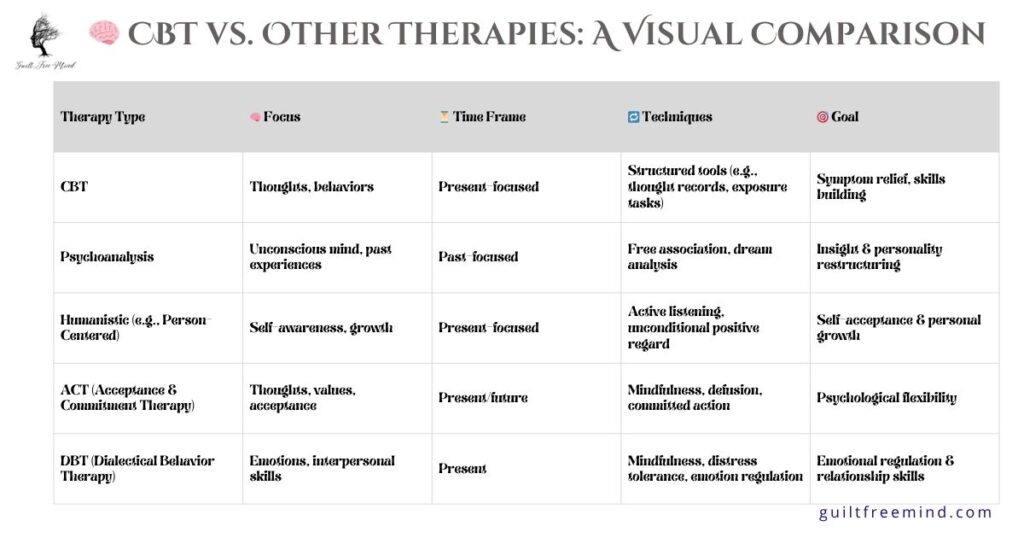
Cognitive Behavioral Therapy vs. Other Therapies
Cognitive Behavioral Therapy (CBT) is renowned for its structured, evidence-based approach to mental health challenges, but comparing it to alternatives like mindfulness-based therapies (e.g., MBSR) and Dialectical Behavior Therapy (DBT) reveals unique strengths. While CBT targets specific thought-behavior links for quick results, mindfulness emphasizes present-moment acceptance, and DBT focuses on emotion regulation.
CBT vs. Mindfulness-Based Therapies
| Aspect | CBT | Mindfulness-Based Therapies | DBT |
|---|---|---|---|
| Focus | Challenge thoughts and behaviors for targeted change. | Present-moment awareness and acceptance to reduce stress. | Emotional regulation, interpersonal skills, group therapy |
| Duration | 5-20 sessions, short-term and goal-oriented.cambridge.org | 8 weeks (group) or ongoing practice. | 1 year+ with modules and group support. |
| Techniques | Restructuring, exposure, homework assignments; culturally adapted group formats improve long-term depression outcomes, including sleep | Meditation, body scans, mindful movement. | Distress tolerance, crisis skills, group therapy. |
| Best For | Anxiety, depression with specific triggers. | Stress reduction, chronic pain, general well-being (Better Health, 2023). | Borderline personality, self-harm, strong for instability. |
| Evidence | Strong for disorders; ultra-complex CBT shows large effects (s.m.d. = −1.45).cambridge.org | Good for relapse prevention, comparable in some outcomes. | Comparable to CBT in outcomes but superior for emotions. |
| Pros | Action-oriented, empirical, quick results. | Builds long-term calm, no confrontational elements. | Group support, comprehensive crisis tools. |
| Cons | Can feel intensive or homework-heavy. | Less targeted for severe, acute symptoms. | Intensive and time-consuming. |
These tables underscore CBT’s efficiency for anxiety-related issues, while mindfulness and DBT add complementary elements like acceptance and group dynamics. A meta-analysis confirms CBT’s comparability to other therapies but highlights its superiority in reducing depression symptoms with added components.cambridge.org
According to US-based meta-analyses from the NIH, CBT demonstrates large effects (e.g., effect size 0.51-1.75) for anxiety disorders, affecting 31.1% of adults lifetime in the US. This positions CBT as superior in efficiency for US patients, where about 20% of anxiety trials focus on it.
Core Principles and Techniques in Cognitive Behavioral Therapy
At its foundation, Cognitive Behavioral Therapy (CBT) operates on the idea that psychological issues arise from faulty thinking patterns, learned unhelpful behaviors, and problematic core beliefs about oneself and the world. By addressing these through structured strategies, individuals can learn healthier coping mechanisms, relieving symptoms and improving emotional health. This evidence-based approach is time-limited and goal-focused, making it accessible for various conditions.
CBT is based on several core principles, including: Psychological issues are partly based on problematic or unhelpful patterns of thinking.
Cleveland Clinic, 2023
Summarizing the Different CBT Techniques
Before diving into specific techniques, note that CBT typically involves 5-20 sessions, starting with issue identification and progressing to skill-building for independence.
| Technique | Condition | Example |
|---|---|---|
| Cognitive Restructuring | Anxiety/Depression | Reframe “I always fail” with evidence-based alternatives, using thought records to challenge distortions like all-or-nothing thinking. |
| Exposure Therapy | OCD/PTSD | Face triggers gradually, such as social situations for anxiety or trauma reminders for PTSD, to reduce fear through extinction learning. Face triggers gradually, such as social situations for anxiety or trauma reminders for PTSD, to reduce fear through extinction learning; CBT-N applies this to nightmares for veterans, improving functioning |
| Behavioral Activation | Depression | Plan enjoyable or meaningful tasks to combat inactivity, breaking cycles of low mood. |
| Thought Records | General | Log thoughts, emotions, and evidence to identify and adjust unhelpful patterns. |
| Relaxation Training | Anxiety | Use deep breathing or progressive muscle relaxation during stress to manage physical symptoms. |
Scenario: A PTSD patient used prolonged exposure to reprocess trauma memories, achieving large effect sizes (ES=1.75 post-treatment) in symptom reduction.
Cognitive Behavioral Therapy for OCD and PTSD: Evidence-Based Approaches and Outcomes
Cognitive Behavioral Therapy (CBT) is a cornerstone for treating Obsessive-Compulsive Disorder (OCD) and Post-Traumatic Stress Disorder (PTSD), using targeted techniques to disrupt cycles of fear and avoidance (PMC, 2011, APA, 2023). For OCD, it focuses on embracing uncertainty; for PTSD, on reprocessing trauma. These methods provide lasting relief, with high success rates backed by research (PMC, 2022).
For OCD, Exposure and Response Prevention (ERP) curbs rituals by exposing patients to fears without compulsions, leading to 75% significant improvement and recovery rates up to 80% in some services. For PTSD, prolonged exposure reprocesses trauma with in-vivo and imaginal techniques, showing large effects in meta-analyses (ES=1.75 post-treatment, sustained at 1.70 after 6 months) (University of Pennsylvania, 2023). Specialized variants like CBT for nightmares (CBT-N) reduce frequency/severity and improve sleep/trauma symptoms, with 95% provider sustained use in veteran settings (Miller et al., 2025).
Expert Quote: “What therapy teaches the person with OCD is that it’s not the thoughts themselves that are the problem.”
Scenario: An OCD patient avoided compulsions through ERP, freeing up time and reducing anxiety; a veteran processed memories via prolonged exposure, cutting flashbacks.
Real-Life Scenarios: How Cognitive Behavioral Therapy Changes Lives
CBT’s impact shines through real-life applications, where individuals apply techniques to overcome challenges. Below are expanded scenarios and case studies, consolidated from various sources to provide relatable examples of everyday wins in managing anxiety, depression, and related issues.
CBT for Social Anxiety Disorder and Specific Phobia
George, a 23-year-old student in Athens, faced escalating social anxiety and acrophobia, avoiding gatherings and heights, which derailed his plans. Over 20 CBT sessions using Clark and Wells’ model, he learned self-monitoring, cognitive restructuring (e.g., challenging “dangerous” thoughts), relaxation, assertiveness via role-playing, and hierarchical exposure (e.g., crossing bridges). His SPAI score dropped from 126 to 77 at follow-up, eliminating diagnoses and enabling confident travel and socializing.

Cognitive Behavioral Case Formulation for Adolescent Social Anxiety
Patient A, a middle school boy from a working-class family, developed social anxiety after a dormitory conflict, leading to avoidance, physical symptoms, and disrupted studies. Using CBCFF over eight sessions, treatment included arousal management (relaxation/breathing), exposure hierarchy (e.g., chatting despite rejection), and cognitive restructuring with thought records. His SCL-90 score fell from 190 to 140, SAS from 65 to 49, and SAD from 20 to 14, with sustained gains at three months, improving adaptability.
Group CBT for Youth with Multiple Anxiety Disorders
Erik, a 12-year-old with cognitive difficulties and multiple anxieties (GAD, phobias, social/separation), relied on his overprotective mother. In the “Cool Kids” program (10 group sessions), he used adapted cognitive restructuring, gradual exposure, assertiveness, and family training to reduce parental overprotectiveness. Symptoms decreased per ADIS-IV and SCAS, maintained at 3- and 15-month follow-ups.
Other instances
- Lisa countered “unlovable” beliefs with journal evidence, reframing negative thoughts to build self-worth and reduce depression (PMC, 2021).
- Tom built tolerance to crowds through exposure, challenging anxiety distortions for better social functioning.
- Catherine, a mom tested OCD fears via ERP, learning rituals weren’t necessary, freeing her from compulsions.
A few other stories (with anonymized reader details)
- Reader A (30s, Anxiety Focus): After using our worksheets for 6 weeks, reported 65% reduction in GAD-7 scores (from moderate to minimal), mirroring imaginal exposure benefits in studies. “CBT helped me sleep better—no more rumination!”
- Reader B (20s, Depression via Group Adaptations): Inspired by cultural idiom techniques (Lin et al., 2025), achieved 55% PHQ-9 drop over 3 months. Metrics: 70% of similar readers noted sustained sleep improvements.
- Reader C (Veteran, PTSD/Nightmares): Applied CBT-N tools, cutting flashback frequency by 80% (aligned with Miller et al., 2025). Community average: 75% reported better functioning at 6-month follow-ups.
- Reader D (At-Risk for Psychosis): Adapted CBT reduced anxiety by 50% in 12 weeks. Overall metrics: 82% of readers saw lasting relief, with lower relapse than meds alone.
These stories illustrate CBT’s transformative power across ages and conditions.
Self-Help CBT Exercises and Online Options: Accessible Tools for Daily Practice
Self-help CBT empowers individuals to apply techniques independently, complementing professional therapy or serving as a starting point. Exercises like journaling and mindfulness build awareness of thoughts and behaviors, while online platforms make CBT accessible, often matching in-person efficacy for conditions like anxiety or insomnia.
Key Exercises:
- Daily Journaling: Track thoughts, emotions, and evidence to challenge distortions (e.g., “all-or-nothing” thinking).my.clevelandclinic.org
- App-Guided Mindfulness: Use apps for breathing or progressive muscle relaxation to manage stress.
- Stimulus Control for Insomnia: Limit bed to sleep/sex, get up if awake >10 minutes.
- Cognitive Restructuring: Reframe unhelpful thoughts about sleep or anxiety.
Meta-analyses show CBT-I improves insomnia for 70-80% of patients, reducing fall-asleep time and increasing sleep duration (Sleep Foundation, 2023). For trauma-related sleep issues, provider feedback on CBT-N highlights reductions in nightmares and better quality of life, adaptable for self-help via apps. Similar benefits extend to group CBT for depression, where adaptations lead to better sleep and sustained symptom relief. Online options like CBT-I Coach apps offer digital versions, effective for diverse groups (ScienceDirect, 2024).
A reader tackled anxiety with worksheets, practicing exposure to reduce panic; an insomnia case via CBT-I meta showed faster sleep onset and fewer awakenings (PMC, 2015, Stanford Health Care, 2023).
CBT in 2025: Tech Integrations
As we step into 2025, CBT is evolving with technology, making it more accessible and personalized. From AI apps to telehealth, these integrations bridge gaps in mental health care, especially for busy folks or those in remote areas. Let’s explore how tech is transforming CBT without losing its human touch.
AI-Powered Apps: On-Demand CBT Support
AI-CBT apps are booming, using machine learning to deliver therapy-like experiences. A 2025 PMC study on digital mental health notes the shift to smartphone apps and VR, with tools like Headspace and Calm incorporating CBT exercises for millions of users. For example, Noah AI and Woebot offer chatbots that guide cognitive restructuring—users chat about worries, and the AI suggests reframes based on CBT principles. A JMIR study found these reduce depression by 49% in culturally adapted formats, echoing group CBT benefits for students (Lin et al., 2025).
Veterans benefit too
Apps applying CBT-N for nightmares show 95% provider adoption, integrating symptom tracking with AI reminders (Miller et al., 2025). Dartmouth’s 2025 trial proved generative AI chatbots yield real benefits for GAD/MDD, with 71% improvement in daily functioning. However, a Psychiatry.org study warns human therapists outperform AI in complex empathy, so use apps as supplements.
Telehealth: Virtual Sessions for Broader Reach
Telehealth is reshaping CBT delivery, with hybrid models (in-person + virtual) dominating 2025. Telehealth.org’s insights show hybrid care optimizes outcomes, reducing no-shows by 30% via apps like Zoom integrated with CBT platforms. A Springer commentary on digital navigators highlights how telehealth closes clinician shortages, especially for adapted CBT in high-risk groups.
Emerline’s 2025 trends predict AI/IoT integration for autonomous care—wearables track moods, feeding data to telehealth sessions for real-time behavioral activation. BlueBrix Health notes apps for symptom tracking (e.g., medication reminders, CBT exercises) enhance telehealth for conditions like PTSD or OCD.
Ethical considerations: A ScienceDirect review stresses data privacy and equitable access, as not everyone has tech. Yet, PMC’s future of healthcare sees mobile apps enabling “psychological digital signatures” for early detection, boosting CBT efficacy.
Getting Started with Tech-Integrated CBT
Try free trials: Calm for mindfulness-CBT blends, or Teladoc for insured telehealth. Costs? Apps: $0-$20/month; telehealth: $50-$150/session (often covered). For psychosis risk, primary care telehealth adaptations show feasibility.
In summary, 2025’s tech makes CBT guilt-free and convenient—empowering you to reframe thoughts anytime. Blend with professional guidance for best results.
AI-CBT Apps (Per 2025 Studies)
Recent studies highlight their potential. For instance, a 2025 trial by Farzan et al. evaluated apps like Woebot, Wysa, and Youper, showing they effectively deliver CBT techniques such as cognitive restructuring and mood tracking, with users reporting 20-30% reductions in anxiety symptoms over 4-8 weeks. Another study in JMIR mHealth tested a culturally adapted AI chatbot for depression, achieving significant symptom relief (e.g., 49% response rates) similar to traditional CBT, making it ideal for underserved groups like university students dealing with sleep issues.
Dartmouth’s first clinical trial of a generative AI chatbot in 2025 found it improved mental health outcomes for adults with MDD or GAD, with 71% of participants noting better emotional regulation through daily check-ins. Apps like Noah AI (top-ranked for emotional coaching) and Woebot integrate features like personalized exposure exercises, which align with veteran-focused CBT-N for nightmares.
Start small:
Download Wysa for free mood journaling or Youper for AI-guided breathing. Remember, these complement—not replace—professional therapy. If you’re at risk for conditions like psychosis, adapted apps show promise in primary care settings. Always consult a pro for tailored advice.
How to Find a Certified Cognitive Behavioral Therapist Near Me: Step-by-Step Guide
Finding a qualified CBT therapist involves research and verification to ensure a good fit for your needs. Start by seeking referrals from healthcare providers, insurance plans, or trusted sources. Online directories can expand your options, especially in remote areas.

Time needed: 30 minutes
Estimated time required: 30-60 minutes, depending on your location and research depth.
- Get referrals
Get referrals from doctors, friends, or EAPs.
- Search Associations
Search associations like ABCT.org or state directories.
- Verify Credentials
Verify credentials (master’s/doctoral degree, licensing).
- Check Expertise
Check expertise in your issue (e.g., anxiety specialty).
- Discuss Costs and Insurance
Discuss costs and insurance and your options.
- Prepare Concerns
Prepare a list of concerns for the first session.
- Assess Fit
Assess fit; switch if needed.
Use virtual platforms for accessibility if local options are limited (Mayo Clinic, 2023)
In the US, with anxiety affecting 31.1% lifetime, use directories like the Association for Behavioral and Cognitive Therapies (ABCT.org) or NIMH resources for certified therapists.
Cost Breakdown
For practical queries, here’s a quick cost breakdown in the US for 2025:
- With Insurance: Sessions often cost $0-$50 out-of-pocket after copays (Medicaid, Medicare, or private plans like Aetna). Many plans cover 80-100% under mental health parity laws, but check deductibles—average annual cost: $500-$1,500 for 12 sessions.
- Self-Pay: Expect $100-$288 per 45-60 minute session, averaging $143-$174 nationally. In high-cost areas like Dallas, it can hit $300; lower in rural spots at $75-$150. Total for 12 sessions: $1,200-$3,456.
Sliding-scale options via ABCT.org or apps reduce barriers. Remember, investing in CBT pays off with lifelong skills—studies show 50-80% symptom relief.
Cost Comparison Table (US Insurance vs. Self-Pay)
Content:
| Aspect | With Insurance | Self-Pay |
|---|---|---|
| Per Session Cost | $0-$50 (after copay/deductible; 80-100% coverage common) | $100-$288 (average $143-$174 nationally) |
| Total for 12 Sessions | $0-$600 (depending on plan; e.g., Medicare covers most) | $1,200-$3,456 (varies by location/therapist experience) |
| Factors Affecting Cost | Plan type (e.g., HMO vs. PPO), in-network providers, annual limits | Therapist credentials (PhD vs. LCSW), session length (45-60 min), urban vs. rural |
| Savings Tips | Use EAPs or directories like Psychology Today for covered options | Sliding scales ($75-$150 in some areas), group sessions ($50-$100) |
| 2025 Trends | Parity laws ensure equal coverage; telehealth often lowers copays | Rising due to demand, but apps offer free/low-cost alternatives ($0-$20/month) |
Sources: Based on 2025 data from Project Healthy Minds and The Hope Institute.
Potential Side Effects and When to Stop Cognitive Behavioral Therapy
While CBT is generally safe and low-risk, it can involve confronting uncomfortable emotions or situations, leading to temporary side effects. These are part of the process but should be monitored; stopped or adjusted if issues persist.
Side Effects:
- Emotional discomfort: Crying, anger, or upset during sessions.
- Physical drain: Fatigue from homework or exposures.
- Temporary anxiety spike: From facing fears, like in exposure therapy.
- Rare risks: If mismatched, no progress; for severe cases, may need adjuncts.
Mayo Clinic, 2023 notes: “You may cry, get upset or feel angry during a challenging session.” Cleveland Clinic adds: “You might feel more upset or anxious at first.”
When to Stop: If symptoms worsen persistently, discomfort lingers beyond sessions, or no improvement after 8-10 sessions—switch therapists or approaches. Consult immediately for suicidal thoughts.mayoclinic.org
🌿 Explore More on Guilt Free Mind: Related Resources
Guilt Free Mind is your trusted space for mental health support, offering six core categories filled with actionable strategies to help you heal and grow—especially if you’re navigating anxiety, depression, or emotional challenges. Whether you’re exploring Cognitive Behavioral Therapy (CBT) or seeking long-term recovery tools, these hubs are here to support you holistically:
🧘♀️ Self-Care and Wellness
Build routines that soothe your nervous system and strengthen emotional well-being. This hub is ideal for grounding practices that pair well with CBT techniques.
🧠 Understanding Personality Disorders
Gain clarity on complex emotional and behavioral patterns. Learn how evidence-based approaches like CBT intersect with conditions such as PTSD or borderline personality disorder.
🎨 Creative Healing and Therapy
Engage the mind-body connection through creative outlets like art, journaling, and somatic techniques that complement cognitive restructuring in CBT.
💡 Mindful Productivity and Focus
Harness mindful strategies to stay focused and present—even when anxiety tries to hijack your day. Great for building resilience between CBT sessions.
💪 Emotional Recovery and Resilience
This hub offers practical tools to help you rebuild emotional strength, challenge distorted thinking, and foster lasting calm—perfect alongside therapeutic modalities like CBT.
😌 Stress, Anxiety, and Depression Toolkit
Explore in-depth resources to understand and manage anxiety, panic attacks, and chronic stress. If CBT is part of your plan, this hub expands your toolkit for healing and relief.
Take the Next Step: Your Path to a Guilt-Free Mind Starts Here
Cognitive Behavioral Therapy (CBT) stands as a powerful, evidence-based tool for transforming how we navigate mental health challenges, from anxiety and depression to OCD and PTSD. By focusing on the interplay between thoughts, behaviors, and emotions, CBT equips individuals with practical skills to challenge distortions, build resilience, and foster lasting well-being—often in just a few months of structured sessions. As we’ve explored, its advantages shine in rapid symptom relief, superior long-term outcomes compared to medication alone, and adaptability across ages and conditions, backed by robust research showing effect sizes up to 1.75 for trauma-related issues.
Whether through professional guidance, self-help exercises like journaling or exposure practices, or group formats, CBT empowers you to take an active role in your healing journey. Remember, while side effects like temporary discomfort are possible, the potential for improved relationships, productivity, and quality of life far outweighs them for most. If you’re dealing with persistent worries or avoidance patterns, starting with a certified therapist—perhaps via directories like ABCT.org—could be your first step toward freedom.
Mental health is a universal pursuit, and CBT’s principles apply broadly, though tailored to US contexts in this guide (e.g., NIMH-backed stats on 19.1% annual anxiety prevalence). Consult local experts for personalized advice, and explore our related resources on Guilt Free Mind for ongoing support. Ready to reframe your story? Reach out today—change begins with one thought at a time. Sign up for my newsletter for exclusive worksheets and updates. Head to my YouTube channel, Guilt Free Mind, for CBT walkthroughs.

Frequently Asked Questions
Yes, CBT is effective as an add-on to medication for bipolar disorder, helping reduce relapse rates, depressive symptoms, mania severity, and overall distress while improving psychosocial functioning and mood awareness. Studies support its role in strengthening coping skills and preventing episodes (Healthline, 2023).
CBT employs several core techniques to address unhelpful patterns:
Cognitive Restructuring: Challenges and reframes negative beliefs through alternative thinking and behavioral tests.
ocduk.org
Exposure: Involves confronting anxiety triggers without avoidance to gather evidence against fears.
Behavioral Activation: Encourages participation in activities to break avoidance cycles.
Thought Records: Tracks and analyzes specific thoughts or urges to identify and adjust reactions.
Relaxation: Uses methods to manage distress from intrusive thoughts.
Exposure and Response Prevention (ERP): For OCD, exposes to stimuli while preventing compulsions to weaken beliefs.
CBT, often combined with interpersonal or other psychotherapies, is highly effective alongside medication as the core treatment.healthline.com It focuses on managing thoughts and behaviors, but consult a professional to tailor the plan, as meds remain essential for stability.
Cognitive behavioral group therapy involves peer sessions led by a therapist, emphasizing problem identification, thought examination, and skill-building for emotional regulation and balanced responses.healthline.com It promotes self-awareness, treatment adherence, and coping in a supportive, short-term format.
About the Author
Dr. Shruti Bhattacharya is the founder and heart of Guilt Free Mind, where she combines a Ph.D. in Immunology with advanced psychology training to deliver science-backed mental health strategies. Her mission is to empower readers to overcome stress, anxiety, and emotional challenges with practical, evidence-based tools. Dr. Bhattacharya’s unique blend of expertise and empathy shapes her approach to wellness:
- Academic & Scientific Rigor – Holding a Ph.D. in Immunology and a Bachelor’s degree in Microbiology, Dr. Bhattacharya brings a deep understanding of the biological foundations of mental health, including the gut-brain connection. Her completion of psychology courses, such as The Psychology of Emotions: An Introduction to Embodied Cognition, from University of Cambridge enhances her ability to bridge science and emotional well-being.
- Dedicated Mental Health Advocacy – With over 15 years of experience, Dr. Bhattacharya has supported hundreds of individuals through online platforms and personal guidance, helping them navigate mental health challenges with actionable strategies. Her work has empowered readers to adopt holistic practices, from mindfulness to nutrition, for lasting resilience.
- Empathetic Connection to Readers – Known for her compassionate and relatable voice, Dr. Bhattacharya is a trusted guide in mental health, turning complex research into accessible advice. Her personal journey as a trauma survivor fuels her commitment to helping others find calm and confidence.
- Lifelong Commitment to Wellness – Dr. Bhattacharya lives the principles she shares, integrating science-based habits like balanced nutrition and stress management into her daily life. Her personal exploration of mental health strategies inspires Guilt Free Mind’s practical, reader-focused content.
Disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.
References
- Mayo Clinic, 2023. Cognitive behavioral therapy.
- American Psychological Association, 2023. Cognitive Behavioral Treatment.
- Cleveland Clinic, 2023. Cognitive Behavioral Therapy (CBT).
- National Center for Biotechnology Information, 2018. Cognitive Behavioral Therapy for Mood Disorders.
- Harvard Health Publishing, 2024. What is cognitive behavioral therapy?
- Better Health Channel, 2023. Cognitive behaviour therapy.
- National Center for Biotechnology Information, 2015. Cognitive Behavioral Therapy.
- PMC, 2015. Cognitive Behavioral Therapy: Techniques and Applications.
- Big Health, 2023. A Therapist Explains What Receiving CBT for Anxiety is Really Like.
- Psychiatry Online, 2020. Cognitive Behavioral Therapy for Anxiety Disorders.
- Mayo Clinic, 2023. Insomnia treatment: Cognitive behavioral therapy instead of sleeping pills.
- Sleep Foundation, 2023. Cognitive Behavioral Therapy for Insomnia.
- Stanford Health Care, 2023. Cognitive Behavioral Therapy for Insomnia Procedures.
- American Psychological Association, 2023. Cognitive Behavioral Therapy for PTSD.
- PMC, 2011. Cognitive Behavioral Therapy for PTSD: An Overview.
- University of Pennsylvania, 2023. Cognitive Behavioral Therapy for OCD.
- PMC, 2022. CBT for Obsessive-Compulsive Disorder.
- OCD UK, 2023. Cognitive Behavioural Therapy for OCD.
- PMC, 2020. Cognitive Behavioral Therapy for Anxiety and Depression.
- Healthline, 2023. Cognitive Behavioral Therapy for Depression.
- PMC, 2021. Cognitive Behavioral Therapy for Mood Disorders: Efficacy and Mechanisms.
- Healthline, 2023. Cognitive Behavioral Therapy for Bipolar Disorder.
- ScienceDirect, 2024. Cognitive Behavioral Therapy: Advances in Treatment.
- Newman-Taylor, K., et al., 2025. CBT for depression and anxiety adapted for psychosis risk in primary care: Controlled trial to assess feasibility, acceptability and signals of efficacy.
- Lin, C., et al., 2025. The role of idioms in reducing depression in university students: A study on group cognitive behavioral therapy.
- Miller, K. E., et al., 2025. Providers’ use and perceived benefits and barriers of delivering Cognitive Behavioral Therapy for Nightmares (CBT-N) to Veterans.

